Experience the OCT difference.
Request your Abbott Sales rep today.
What is Optical Coherence Tomography (OCT) Imaging?
Optical Coherence Tomography (OCT) is an intravascular imaging modality that uses near-infrared light to provide high-definition, cross-sectional and three-dimensional images of the vessel microstructure.
These images provide additional information on the degree and characteristics of coronary artery disease compared to angiography, which doesn’t delineate the composition of the coronary artery.1 With automated, highly accurate measurements, OCT can guide stent selection, placement, and deployment.1
OCT Software — Intuitive User-Interface
Ultreon™ 2.0 Software is powered by artificial intelligence (AI) and automation. Ultreon™ 2.0 Software features an improved user interface that balances simplicity of display with access to powerful analysis.

Ultreon™ 2.0 Software User Interface. Pre-PCI OCT pullback: Integration of AI-powered insights to your angiography panel helps identify calcified plaque.
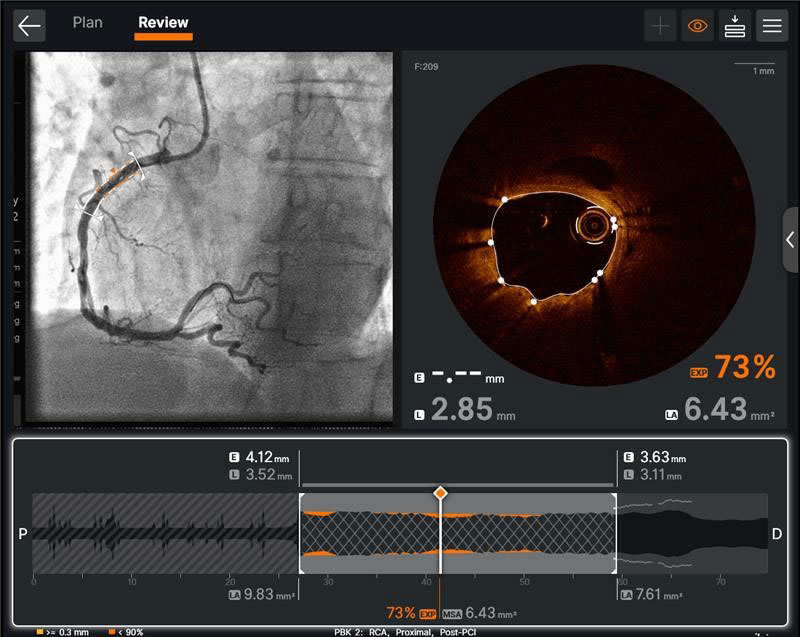
Ultreon™ 2.0 Software User Interface. Post-PCI OCT pullback: The OCT software provides post-PCI analysis to support optimization of deployed stent.
How does OCT support PCI guidance?
- For pre-PCI guidance, OCT can be used to identify the culprit lesion, assess lesion morphology to select the right lesion preparation strategy, and characterize the stent landing zones to select precise length and diameter of balloons and stents.2
- For post-PCI guidance, OCT offers improved visualization of stent dissection, tissue protrusion and incomplete vessel wall apposition compared to angiography alone, thus helping to minimize stent thrombosis.3 OCT helps to confirm that stent is fully expanded to reduce stent failure.1
PCI guidance with OCT is easy with the standardized step-by-step workflow, MLD MAX, which is the mnemonic for Morphology, Length, Diameter, Medial Dissection, Apposition and Xpansion.4,5 Using OCT with MLD MAX workflow can optimize stent delivery by improving expansion and minimizing malapposition5 without additional contrast while reducing radiation exposure compared to angiography-guided PCI.6 Optimized stent expansion is linked to better PCI outcomes.7
OCT has Class 1A Recommendations for Both ACS and CCS
2024 ESC Guidelines for CCS
OCT is included in the revascularization treatment for complex PCI with Class 1A recommendation; especially in left main stem, true bifurcation, and long lesions.8
2025 AHA/ACC Guidelines for ACS
OCT received a Class 1A recommendation in patients with acute coronary syndromes undergoing coronary stent implantation in left main artery or in complex lesions.9
The Basics of Optical Coherence Tomography
What are the components of OCT?
OCT imaging systems consists of three main components: the software, the system, and the catheter.
OCT Software
Ultreon™ 2.0 Software includes automatic detection of vessel morphologies based on artificial intelligence. The software is intended to be used only with compatible OPTIS™ Next Imaging Systems.

OPTIS™ Next Imaging Systems
The hardware that runs the OCT software. OPTIS™ Next Systems use optical imaging catheters that emit near-infrared light to produce high-resolution real-time images. The OPTIS™ Next Imaging Systems can be integrated with the cath lab angio systems to display OCT and angio co-registration (ACR) on the same screen.

OCT Catheter
The Dragonfly OpStar™ Imaging Catheter is intended for the imaging of coronary arteries.

OCT Image Acquisition and Interpretation
To create an OCT scan, an OCT catheter is inserted into the vessel and an infrared laser is used to scan the vessel wall in a spiral-like manner. The laser beam penetrates the tissue, is reflected from there and returned to the OCT device via the catheter for evaluation.10
How to set up the system for OCT-guided PCI
Watch this video to learn how to set up the OCT system.
There are four steps to an OCT-guided PCI set up:2
- Connecting syringe
- Purging the catheter
- Draping the DOC
- Connecting the catheter
How to initiate a pullback
Watch this video to learn how to initiate a pullback. The step-by-step instructions are also available on the OCT screen.
Due to the OCT systems’ high acquisition speed, images of pullback can be produced and visualized in a matter of seconds. The system provides precise information about the scanned vessel segment.10
How to interpret OCT images
Learn how to interpret OCT images, the basic elements of an OCT image, and a workflow for image interpretation.
OCT and MLD MAX Workflow
Using OCT with MLD MAX workflow, the standardized step-by-step workflow, helps to guide pre- and post-PCI decisions. Use of the workflow resulted in an 86% change in treatment decisions11 compared to angiography alone without a change in contrast usage and a 10% reduction in radiation6, as shown in the LightLab Clinical Initiative.
Six letters represent six steps of the PCI goal to maximize stent expansion to deliver optimal results.
- The first three steps, MLD (Morphology, Length, Diameter) performed before PCI, designed to help inform treatment strategy.
- The last three steps, MAX (Medial Dissection, Apposition, Xpansion), performed post-PCI, to optimize stent placement. MLD MAX was developed as a part of the LightLab Clinical Initiative.
Achieving optimal expansion is proven to reduce rates of major adverse cardiac events during PCI.12 Proper expansion confirmed by imaging results in safety and efficacy benefits.7
Morphology
Search for High Calcium1
Criteria:
>180 degrees, and
>0.5 mm thickness, and
>5 mm in length
Length
Select Landing Zones Based on Healthy Tissue/ EEL Visualization2
Place landing zones in healthy tissue (i.e. EEL visualization)
Note: In the absence of EEL to represent healthy tissue find the largest lumen to avoid areas of TCFA or lipid pools so as to not land your stent edge in these high-risk areas3
Diameter
Measure Vessel,
Stent, Balloon Diameters4
Use distal reference measurements to select stent diameter
Use distal reference measurement for distal balloons or proximal reference measurements for proximal balloons
Medial
Dissection
Address Significant Dissection2,5
Criteria:
Dissection penetrates medial layer, and is greater than 1 quadrant arc
Apposition
Address Gross Malapposition
Criteria:
Malapposition indicator shows longer than 3 mm4 of significant (≥0.3 mm from wall6) apposition
Xpansion
Confirm
Expansion3,7
Criteria:
≥80% acceptable,
≥90% expansion is optimal
“When we use the OCT workflow (MLD MAX), we make better decisions initially by analyzing the plaque morphology and determining appropriate vessel prep as well as selecting the appropriate stent length and diameter. By doing this, we are less likely to have to do post-PCI optimization because we are doing it right the first time. This often leads to improved procedural efficiency.”
— DR. JASON WOLLMUTH, INTERVENTIONAL CARDIOLOGIST
How to Apply MLD MAX Workflow to OCT-Guided PCI?
Watch these videos to learn more about each step of the MLD MAX workflow: Morphology, Length, Diameter, Medial dissection, Apposition, and Xpansion.
Pre-PCI Guidance: MLD | Morphology, Length, Diameter are used to determine PCI strategy.
Morphology
What is the value of morphology-guided lesion prep?
- Understanding vessel morphology and plaque characteristics (lipidic, fibrotic or calcific) helps to determine vessel preparation strategy (e.g., whether to proceed with direct stenting or if plaque modification is required).
- In this video, Dr. Ziad Ali provides a detailed overview of the structure of the normal vessel morphology, how it displays on OCT, and shares an easy-to-use OCT image interpretation workflow.
- Dr. Ziad Ali discusses vessel preparation strategies based on plaque type, and the influence on coronary calcium on stent expansion. Learn more about OCT in calcified lesions.
Length
Why does proper stent length matter?
Diameter
Why does accurate diameter matter?
- Appropriate sizing of stent diameter is important to limit underexpansion, malapposition and dissections.
- Angiography both over- and underestimates stent diameter to a similar degree and led to an inaccurate stent diameter in 37% of stented lesions as demonstrated in the LightLab Clinical Initiative.11
- In this video, Dr. Ziad Ali shows how to measure diameter with an easy-to-use sizing workflow.
Post-PCI Guidance: MAX | Medial dissection, Apposition, Xpansion are used to optimize stent placement to ensure optimal expansion.
Medial Dissection
There are three types of dissections: intimal, medial and intramural hematoma. A medial dissection penetrates the medial layer and is > 1 quadrant arc, with some diagnostic thresholds as low as 60 degrees.5,12
Apposition
What is stent apposition and why does it matter?
Xpansion
An important aspect of optimizing PCI is the detection of underexpansion after stent placement.12
- Underexpansion is a predictor of adverse events, e.g., stent thrombosis and restenosis. Achieving optimal expansion is proven to reduce rates of adverse events.12
- In this video, Dr. Ziad Ali shows how to confirm stent expansion using OCT.
References
*Improved interface as compared to AptiVue™ Software.
- Reyes M, et al. The next innovation in PCI is not a stent. The value of OCT. CathLab Digest. 2019;27(10).
- Ali ZA, et al. Intracoronary optical coherence tomography: state of the art and future directions. EuroIntervention. 2021;17(2):e105-e123.
- Ultreon 2.0 Software Instructions for Use (IFU). Refer to IFU for additional information.
- Cioffi GM, et al. Does artificial intelligence enhance physician interpretation of optical coherence tomography: insights from eye tracking. Front Cardiovasc Med. 2023;10:1283338.
- Shlofmitz E, et al. The MLD MAX OCT Algorithm: an Imaging-based Workflow for Percutaneous Coronary Intervention. Catheter Cardiovasc Interv. 2022;100:S7- S13.
- Osborn EA, et al. Safety and efficiency of percutaneous coronary intervention using a standardised optical coherence tomography workflow. EuroIntervention. 2023;18(14):1178-1187.
- Zhang J, et al. Intravascular ultrasound versus angiography-guided drug-eluting stent implantation: the ULTIMATE trial. JACC. 2018;72(24):3126-3137.
- Vrints C, et al. 2024 ESC guidelines for the management of acute coronary syndromes. European Heart Journal. 2024;45(36):3415-3537.
- Rao S, et al. 2025 ACC/AHA/ACEP/NAEMSP/SCAI Guideline for the Management of Patients With Acute Coronary Syndromes. JACC. 2025;151: e771-e862.
- Johann K, Loblich K. Chapter 1: Systemic OCT image evaluation. In: Nef H, Elsasser A, eds. OCT compendium. 1st ed. Germany.
- Bergmark B, et al. Decision-Making During PCI Guided by OCT: Insights from the LightLab Initiative. Circulation Cardiovasc Interv. 2022;15:e011851.
- Räber L, et al. Clinical use of intracoronary imaging. Part 1: guidance and optimization of coronary interventions. An expert consensus document of the European Association of Percutaneous Cardiovascular Interventions. European Heart Journal. 2018;39(35):3281-3300.
- Prati F, et al. Clinical Impact of OCT Findings During PCI: The CLI-OPCI II study. JACC: Cardiovascular Imaging. 2015;8(11):1297-1305.
References - MLD MAX graphic
- Fujino A, et al. A new optical coherence tomography-based calcium scoring system to predict stent under expansion. EuroIntervention. 2018;13(18):e2182-e2189.
- Prati F, et al. Clinical Impact of OCT Findings During PCI: The CLI-OPCI II study. JACC: Cardiovascular Imaging. 2015;8(11):1297-1305.
- Kubo T, et al. Application of optical coherence tomography in percutaneous coronary intervention. Circulation Journal. 2012;76(9):2076-2083.
- Ali ZA, et al. Optical coherence tomography compared with intravascular ultrasound and with angiography to guide coronary stent implantation (ILUMIEN III: OPTIMIZE PCI): a randomised controlled trial. Lancet. 2016;388(10060):2618-2628.
- Shlofmitz E, et al. The MLD MAX OCT Algorithm: an Imaging-based Workflow for Percutaneous Coronary Intervention. Catheter Cardiovasc Interv. 2022; 100: S7- S13.
- Souteryrand G, et al. Mechanisms of stent thrombosis analysed by optical coherence tomography: insights from the national PESTO French registry. European Heart Journal. 2016;37(15):1208-1216.
- Meneveau N, et al. Optical coherence tomography to optimize results of percutaneous coronary intervention in patients with non–ST-elevation acute coronary syndrome: results of the multicenter, randomized DOCTORS study (does optical coherence tomography optimize results of stenting). European Heart Journal. 2016;134(13):906-17.
MAT-2105101 v3.0