Experience the OCT difference.
Request your Abbott Sales rep today.
OCT-guided PCI Improved Procedural Outcomes and Safety Results compared to Angiography-Guided PCI as Demonstrated in ILUMIEN IV1, OCTOBER2
ILUMIEN IV
ILUMIEN IV is the largest global imaging randomized clinical trial with n=2,487 patients in 80 global centers. The trial compared OCT-guided stent implantation vs. angiography guided in high-risk or complex lesions. Primary endpoint was achieving larger post-PCI lumen dimensions and improving clinical outcomes.
ILUMIEN IV OVERVIEW

KEY RESULTS:
OCT-guided PCI significantly reduced stent thrombosis (ST) by 64%

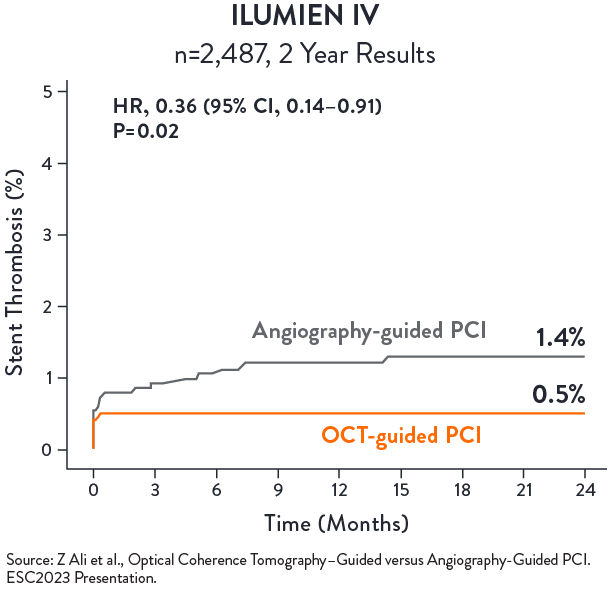
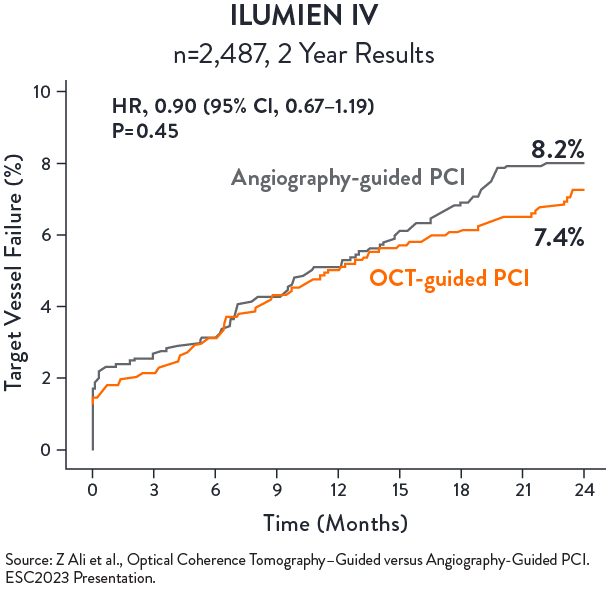
No statistical difference in TVF between OCT-guided and angio-guided PCI at 2 years
ILUMIEN IV SUBSTUDY: COMPLEX LESIONS3
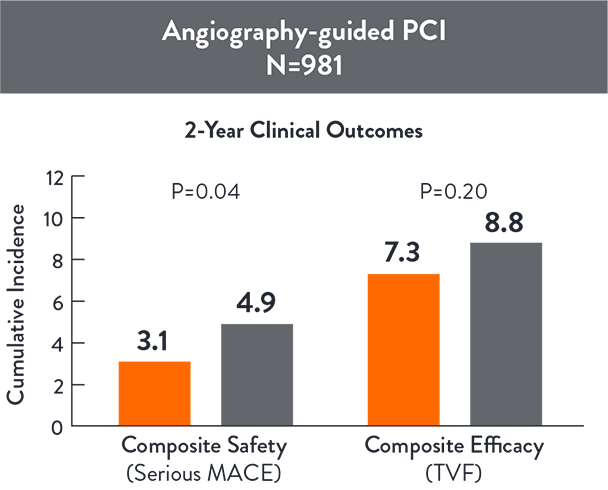
ILUMIEN IV Substudy: Complex Lesions aimed to specifically examine if OCT-guided PCI improves procedural and clinical outcomes compared with angio-guided PCI outcomes in the complex angiographic lesions subgroup (N=1,973)
KEY RESULTS:
OCT-guided PCI reduced serious MACE (Cardiac Death, TV-MI, or Stent Thrombosis) compared with angio-guided PCI at 2 years (p=0.042)3

Source: Ali Z., et al. ILUMIEN IV: OCT-guided vs. angio-guided coronary stent implantation in complex lesions (Sub-group). EuroPCR2024.
Source: Ali Z., et al. ILUMIEN IV: OCT-guided vs. angio-guided coronary stent implantation in complex lesions (Sub-group). EuroPCR2024.
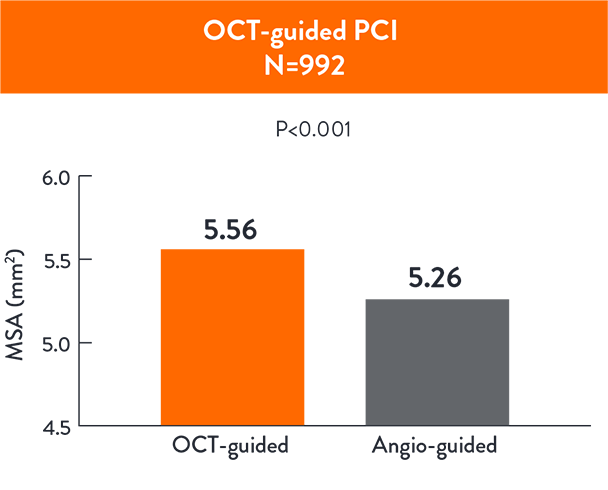
OCT-guided PCI led to a larger MSA ( 5.56 ± 1.95 mm 5.26 ± 1.81 mm2; p< 0.001) compared to angio-guided PCI3

CALIPSO3
CALIPSO Trail (Calcified Lesion Intervention Planning Steered by OCT) is the first controlled randomized trial (n=134) that compared OCT-guided PCI to angio-guided PCI in moderate to severe calcified lesions using pre-defined algorithm for plaque modification, stent sizing and optimization.
- Primary endpoint: post-PCI Minimal Stent Area (MSA) on final OCT
- Secondary endpoints: Efficiency and Safety
KEY RESULTS:
OCT-guided PCI was superior to angio-guided PCI with greater MSA 6.5 (5.5-8.1) vs. 5.0 (4.1-6.1) mm2, p<0.0014.

OCT-guided PCI achieved greater stent expansion and lower malapposition than angio-guided PCI4
| OCT guidance group (n=65) | Angio guidance group (n=69) | p | |
|---|---|---|---|
| Stent length, mm | 33.0 (24.0-48.0) | 38.0 (25.0-48.0) | 0.35 |
| Average stent area, mm2 | 8.4 (7.0-10.3) | 7.4 (6.4-8.6) | 0.01 |
| Successful geometrical expansion, n (%) | 49 (75) | 20 (29) | <0.001 |
| Major malapposition, n (%) | 23 (35) | 34 (49) | 0.10 |
| Malapposition maximal distance, µm | 535 (352-700) | 570 (330-790) | 0.13 |
| Major malapposition length, mm | 0 (0-2) | 0 (0-4) | 0.03 |
| Malapposed stent percentage, % | 0 (0-8.3) | 0 (0-14.5) | 0.02 |
| Average stent eccentricity | 1.21 (1.16-1.25) | 1.19 (1.17-1.24) | 0.87 |
| Maximal stent eccentricity | 1.43 (1.35-1.55) | 1.51 (1.36-1.60) | 0.47 |
| Major dissection, n (%) | 7 (11) | 13 (19) | 0.19 |
Source: Amabile N., et al. OCT vs. angiography for guidance of calcified lesions PCI: the CALIPSO (CAlcified Lesion Intervention Planning Steered by OCT) trial. EuroPCR2024.
No difference in contrast use, procedure time & radiation dose between OCT-guided and angio-guided PCI4
| OCT guidance group (n=65) | Angio guidance group (n=69) | p | |
|---|---|---|---|
| Procedure duration, mins | 63 (51-87) | 64 (46-82) | 0.22 |
| Fluoroscopy duration, mins | 17 (11-21) | 17 (12-27) | 0.95 |
| Total X ray dose, cGy/cm2 | 4148 (2550-7155) | 4403 (2630-7333) | 0.65 |
| Contrast medium volume, ml | 180 (140-233) | 184 (150-219) | 0.88 |
Source: Adapted from Amabile N., et al. OCT vs. angiography for guidance of calcified lesions PCI: the CALIPSO (CAlcified Lesion Intervention Planning Steered by OCT) trial. EuroPCR2024.
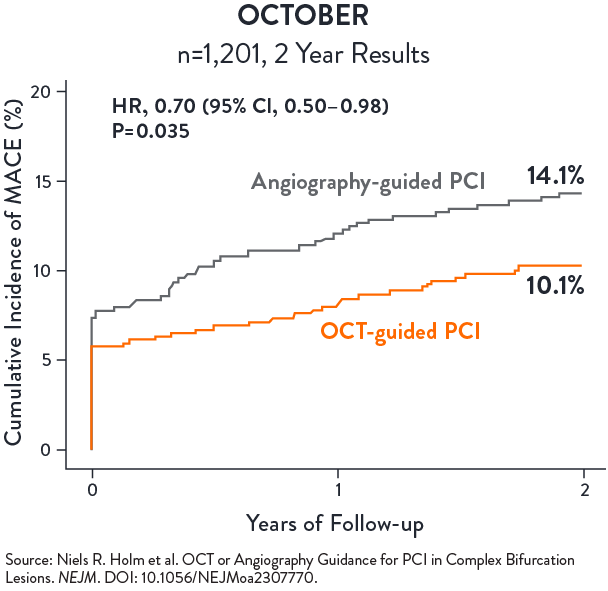
OCTOBER
OCTOBER trial was conducted in 38 heart centres across 13 European countries with n=1,201 patients randomized in a 1:1 ratio to undergo OCT-guided or angiography-guided PCI of bifurcation coronary lesions. A step-wise protocol was use in the OCT arm; in the angiography arm, intravascular ultrasound use was discouraged but could be pursued for left main (LM) PCI.
The primary endpoint was major adverse cardiac events (MACE), defined as a composite of cardiac death, target lesion myocardial infarction (TL-MI), and ischemia-driven target lesion revascularization (ID TLR), after two years.
KEY RESULTS:
OCT-guided PCI of complex bifurcation lesions is superior to angiography-guided PCI for major adverse cardiac events at 2 years2
- MACE @ 2 years:
(10.1% vs 14.1%, p=0.035) - Cardiac death:
1.4% vs. 2.6% (HR 0.53, 95% CI 0.22–1.25) - ID TLR:
2.8% vs. 4.6% (HR 0.60, 95% CI 0.32–1.13) - TL-MI:
7.8% vs. 8.5% (HR 0.90, 95% CI 0.60–1.34)
From Evidence to Practice: A Pragmatic Approach to OCT.
Watch Dr. Johnson demonstrate how to apply OCT-guidance to a complex bifurcation case from a participant in the OCTOBER Trial with a highly challenging left main stent.
Additional body of evidence in support of OCT-guided PCI
Multiple other studies of OCT-guided PCI vs. angiography alone suggest that intravascular imaging with OCT is associated with better clinical performance5,7,9
| STUDY | SIZE | OUTCOMES |
|---|---|---|
| CLI-OPCI I (EuroIntervention, 2012) | 335 pts OCT guided vs 335 pts angio-guided | Reduced rate of cardiac death and MACE in patients who underwent OCT-guided stent intervention.5 |
| ILUMIEN I (EHJ, 2015) | 418 pts | OCT imaging influenced physician decision-making pre-PCI in 57% and post-PCI in 27% of all cases.6 |
| ILUMIEN III (LANCET, 2016) | 450 pts (158 OCT, 146 IVUS, 146 ANGIO) | OCT- guided PCI resulted in superior stent expansion and procedural success compared to angiography-guided PCI.7 |
| DOCTORS (CIRC 2016) | 240 pts NSTEMI | In patients with non-ST-segment elevation acute coronary sydromes, OCT-guided PCI is associated with higher post-procedure FFR than angio-guided PCI.8 |
| PAN-LONDON (JACC CARD INT, 2018) | 1,149 pts OCT, 10,971 pts IVUS 75,046 pts angio | OCT-guided PCI was associated with improved procedural outcomes, in-hospital events and long term survival compared with standard angiography-guided PCI.9 |
References
- Ali Z. et al., Optical Coherence Tomography–Guided versus Angiography-Guided PCI, NEJM, DOI: 10.1056/NEJMoa230586
- Holm N.R. et al., OCT or Angiography Guidance for PCI in Complex Bifurcation Lesions, NEJM, DOI: 10.1056/NEJMoa2307770 (OCTOBER)
- Ali Z., et al. ILUMIEN IV: OCT-guided vs. angio-guided coronary stent implantation in complex lesions (Sub-group). EuroPCR2024.
- Amabile N., et all. OCT vs angiography for guidance of calcified lesions PCI: the CALIPSO trial. EuroPCR 2024
- Prati F. et al. Angiography alone versus angiography plus optical coherence tomography to guide decision-making during percutaneous coronary intervention: (CLI-OPCI) study. EuroIntervention, 2012.
- Wijns W. et al. Optical coherence tomography imaging during percutaneous coronary intervention impacts physician decision-making: ILUMIEN I study. European Heart Journal (2015) 36, 3346–3355 doi:10.1093/eurheartj/ehv367.
- Z. Ali et al. Optical coherence tomography compared with intravascular ultrasound and with angiography to guide coronary stent implantation (ILUMIEN III: OPTIMIZE PCI): a randomised controlled trial. Lancet: https://doi.org/10.1016/S0140-6736(16)31922-5.
- Menevue N. et al. Optical Coherence Tomography to Optimize Results of Percutaneous Coronary Intervention in Patients with Non–ST-Elevation Acute Coronary Syndrome DOCTORS: https://doi.org/10.1161/CIRCULATIONAHA.116.024393 Circulation. 2016;134:906–917.
- Jones, D. et al. Angiography Alone Versus Angiography Plus Optical Coherence Tomography to Guide Percutaneous Coronary Intervention: Outcomes From the Pan-London PCI CohortPan London: JACC Cardiovasc Interv. 2018 Jul 23;11(14):1313-1321. doi: 10.1016/j.jcin.2018.01.274.
MAT-2311283 v3.0
Important Safety Information
OPTIS™ and OPTIS™ Next Imaging Systems and Software

INDICATIONS
Applies to OPTIS™ Imaging Systems and Software
The OPTIS™ Software and AptiVue™ E Series Software are intended to be used only with compatible OPTIS™ Imaging Systems.
The OPTIS™ Imaging Systems with a compatible Dragonfly™ Imaging Catheter are intended for the imaging of coronary arteries and is indicated in patients who are candidates for transluminal interventional procedures. The compatible Dragonfly™ Imaging Catheters are intended for use in vessels 2.0 to 3.5 mm in diameter. The compatible Dragonfly™ Imaging Catheters are not intended for use in the left main coronary artery or in a target vessel which has undergone a previous bypass procedure.
The OPTIS™ Imaging Systems are intended for use in the catheterization and related cardiovascular specialty laboratories and will further compute and display various physiological parameters based on the output from one or more electrodes, transducers, or measuring devices. The physician may use the acquired physiological parameters, along with knowledge of patient history, medical expertise and clinical judgment to determine if therapeutic intervention is indicated.
Applies to OPTIS™ Next Imaging Systems and Software
The Ultreon™ 1.0 Software and Ultreon™ 2.0 Software are intended to be used only with compatible OPTIS™ Next Imaging Systems.
The OPTIS™ Next Imaging System with a compatible Dragonfly™ OPTIS™ Imaging Catheter or Dragonfly OpStar™ Imaging Catheter is intended for the imaging of coronary arteries and is indicated in patients who are candidates for transluminal interventional procedures. The Dragonfly™ OPTIS™ Imaging Catheter or Dragonfly OpStar™ Imaging Catheter is intended for use in vessels 2.0 to 3.5 mm in diameter. The Dragonfly™ OPTIS™ Imaging Catheter or Dragonfly OpStar™ Imaging Catheter is not intended for use in the left main coronary artery or in a target vessel which has undergone a previous bypass procedure.
The OPTIS™ Next Imaging Systems are intended for use in the catheterization and related cardiovascular specialty laboratories and will further compute and display various physiological parameters based on the output from one or more electrodes, transducers, or measuring devices. The physician may use the acquired physiological parameters, along with knowledge of patient history, medical expertise, and clinical judgment to determine if therapeutic intervention is indicated.
Applies to both OPTIS™ and OPTIS™ Next Imaging Systems and Software
The Dragonfly™ OPTIS™ or Dragonfly™ OpStar™ Imaging Catheters are intended for use in vessels 2.0 to 3.5 mm in diameter. The Dragonfly™ OPTIS™ or Dragonfly™ OpStar™ Imaging Catheters are not intended for use in the left main coronary artery or in a target vessel which has undergone a previous bypass procedure.
The OPTIS™ and OPTIS™ Next Imaging Systems are intended for use in the catheterization and related cardiovascular specialty laboratories and will further compute and display various physiological parameters based on the output from one or more electrodes, transducers, or measuring devices. The physician may use the acquired physiological parameters, along with knowledge of patient history, medical expertise, and clinical judgment to determine if therapeutic intervention is indicated.
CONTRAINDICATIONS
The OPTIS™ and OPTIS™ Next Integrated Systems and Mobile Systems with the usage of the OPTIS™ Software, AptiVue™ E Series Software, Ultreon™ 1.0 Software, and Ultreon™ 2.0 Software are contraindicated where introduction of any catheter would constitute a threat to patient safety. Contraindications include:
- Bacteremia or sepsis
- Major coagulation system abnormalities
- Patients diagnosed with coronary artery spasm
- Patients disqualified for coronary artery bypass graft (CABG) surgery
- Patients disqualified for percutaneous transluminal coronary angioplasty (PTCA)
- Severe hemodynamic instability or shock
- Total occlusion
- Large thrombus
- Acute renal failure
- Inability to tolerate systemic anticoagulation is a contraindication to use of OCT for coronary imaging.
- The system has no patient alarm functions. Do not use for cardiac monitoring.
COMPLICATIONS
The following complications may occur as a consequence of intravascular imaging and catheterization procedure:
- Abnormal heart rhythm or arrhythmias
- Acute myocardial infarction
- Allergic reaction to the contrast media or drug administered for the procedure
- Arterial dissection, injury, or perforation
- Bleeding
- Catheter access site reactions: inflammation or granuloma
- Coronary artery spasm
- Death
- Embolism
- Hypotension
- Infection
- Myocardial ischemia
- Renal insufficiency or failure from contrast media use
- Repeat revascularization
- Thrombus formation, abrupt closure, or total occlusion
- Tissue necrosis
- Unstable angina
WARNINGS
- Prior to use, please review the Instructions for Use supplied with the OPTIS™ imaging system, Dragonfly™ Imaging Catheter, Wi-Box™ AO Transmitter and the PressureWire™ guidewire for more information.
- The Dragonfly™ Imaging Catheter is sterilized by ethylene oxide and is intended for one time use only. Non-pyrogenic. Do not use if the package is opened or damaged. Do not reuse or re-sterilize. Any attempt to reuse or re-sterilize may compromise the structural integrity of this device. Adverse effects of using a non-sterile or re-sterilized catheter may include, but are not limited to: local and / or systemic infection, mechanical damage, inaccurate results.
- Appropriate anticoagulant and vasodilator therapy must be used during the procedure as needed.
- Ensure that no air is introduced into the system during the Dragonfly™ Imaging Catheters insertion.
- Observe all advancement and movement of the Dragonfly™ Imaging Catheters under fluoroscopy. Always advance and withdraw the catheter slowly. Failure to observe device movement fluoroscopically may result in vessel injury or device damage. To ensure proper placement, do not move the guide wire after a Dragonfly™ Imaging Catheter is in place.
- If resistance is encountered during advancement or withdrawal of the Dragonfly™ Imaging Catheter, stop manipulation and evaluate under fluoroscopy. If the cause of resistance cannot be determined or mitigated, carefully remove the Dragonfly™ Imaging Catheters and guidewire together as a unit from the patient.
- Leave the guide wire engaged with a Dragonfly™ Imaging Catheter at all times during use. Do not withdraw or advance the guide wire prior to withdrawing the Dragonfly™ Imaging Catheters.
- The Dragonfly™ Imaging Catheters should never be forced into lumens that are narrower than the Dragonfly™ Imaging Catheters body or forced through a tight or heavily calcified lesion.
- The Dragonfly™ Imaging Catheters should not be advanced through abnormally tortuous anatomy.
- When advancing or retracting a Dragonfly™ Imaging Catheter with a monorail tip through a stented vessel, the Dragonfly™ Imaging Catheters may engage the stent between the junction of the Dragonfly™ Imaging Catheters and guide wire, resulting in entrapment of catheter / guide wire, catheter tip separation, stent dislocation, and / or vascular injury.
- Refer to the contrast media Instructions for Use for general warnings and precautions relating to use of contrast media.
- Before creating an OCT recording, review “Performing an OCT Procedure” for additional warnings and cautions in the IFU.
PRECAUTIONS
- Safety and effectiveness have been established for the following patient population: adult patients undergoing non-emergent percutaneous coronary interventions in lesions with reference vessel diameters between 2.0 to 3.5 mm, which are not located in the left main coronary artery or in a target vessel which has undergone previous bypass procedures.
- Follow all instructions, warnings, and cautions provided in “Patient Safety” in the IFU.
- All operators must be knowledgeable in performing OCT and physiological procedures prior to using the OPTIS™ and OPTIS™ Next Integrated Systems and Mobile Systems with the usage of the OPTIS™ Software, AptiVue™ E Series Software, Ultreon™ 1.0 Software, and Ultreon™ 2.0 Software.
- When using saline, heparinized saline is recommended.
- Monitor the OCT image for indications of the Dragonfly™ Imaging Catheters optical failure. If optical failure is suspected, remove the Dragonfly™ Imaging Catheter from the patient, press “Unload” on the drive motor and optical controller (DOC), detach the catheter, and replace it with a new one.
- If the pullback triggers before contrast is injected, repeat the pullback.
- For optimal imaging, only use 100% contrast media.
- Use the minimum flush rate and volume required to image the desired anatomy.
- To obtain accurate measurements, be sure the selection for the Flush Medium is the same as the medium in which you are imaging.
- The Dragonfly™ Imaging Catheters must be purged prior to connection to the DOC to prevent damage to the imaging core.
- Do not insert or remove a Dragonfly™ Imaging Catheter while the DOC is scanning. Do not attempt to disconnect the catheter from the DOC while the “lock” LED is blinking as it could damage the catheter or the DOC. Refer to “Removing the Dragonfly™ Imaging Catheter” in the IFU.
- Never attempt to attach or detach a catheter to the DOC while the "lock" LED is lit.
- Take care in handling the Dragonfly™ Imaging Catheters to prevent breaking the fiber-optics within the catheter. Kinking and bending of the catheter can cause damage. While connecting, ensure the proximal catheter segment is straight and aligned with the DOC. Never attempt to connect and operate the catheter while the catheter remains coiled within the hoop.
- Do not kink, sharply bend, pinch, or crush the Dragonfly™ Imaging Catheters at any time.
- The Dragonfly™ Imaging Catheters have no user serviceable parts. Do not attempt to repair or alter any part of the catheter assembly as provided.
- If you want to make measurements on files that will be exported to standard formats, you must make the measurements BEFORE exporting the images. Using non-OCT software to measure standard format images will not produce accurate measurements.
- Do not use images that have been exported to JPEG or Compressed AVI formats for clinical decision making. These formats use compression methods that may degrade the image quality.
- Artifacts may result in misrepresentation of L-mode data, so L-mode is not recommended for quantification of clinical information.
- It is the user’s responsibility to confirm the lumen contours of all the frames within the reference segment, and to make adjustments if necessary. Red frames indicate low confidence in the detected contours.
- Deleted files cannot be restored. After files have been deleted, they can only be imported back to your system from your archived copies.
- Restoring factory default settings resets ALL user-entered configuration values except the date and time. This button should be used only under the direction of qualified service personnel.
MAT-2309288 v1.0

Stay Connected