Every complex case is unique, and no calcified lesion is the same. That’s why we focus on providing the therapies, tools, and specialized knowledge that enable you to tailor your approach and optimize long-term, durable outcomes.

Individualized Solutions for Calcified Lesions
Our comprehensive portfolio offers individualized solutions for every step in the treatment of calcified lesions from ACCESS to CLOSE.
Access
Gain access with the right guide wires.
Mild Calcification
Moderate Calcification
Severe Calcification
Microcatheters
- Teleport‡
- Teleport‡ Control
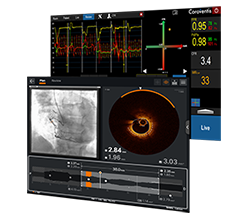
Assess
Visualize the best path forward with OCT and full physiology.
OCT Intravascular Imaging
Epicardial and Microvascular Assessment
Prepare
Clear obstacles with orbital atherectomy and coronary dilatation catheters.
Mild/Moderate Calcification
- Scoreflex‡ NC Scoring PTCA Catheter
- NC TREK NEO™ Coronary Dilatation Catheter
- Sapphire‡ NC24 Coronary Dilatation Catheter
Severe Calcification
Initially Uncrossable Lesion
- Diamondback 360 Precision™ Coronary Orbital Atherectomy System
- Sapphire‡ II PRO 1.0 mm Coronary Dilatation Catheter
- MINI TREK™ and TREK™ Coronary Dilatation Catheters
Scoreflex, Sapphire, and Teleport and OrbusNeich are registered trademarks of OrbusNeich Medical Group Holdings Limited or its affiliates. Manufactured by OrbusNeich Medical Group Holdings Limited or its affiliates. Distributed by Cardiovascular Systems, Inc. (CSI). CSI is a subsidiary of the Abbott Group of Companies.
CAUTION: OrbusNeich products are intended for use by or under the direction of a physician. Prior to use, reference the Instructions for Use at eifu.orbusneich.com for more detailed information on Indications, Contraindications, Warnings, Precautions, and Adverse Events.
MAT-2414252 v2.0
Important Safety Information
HI-TORQUE VERSATURN™ Guide Wire

INDICATIONS FOR USE
This HI-TORQUE™ Guide Wire is intended to facilitate the delivery of catheter-based interventional devices during the following procedures:
- Percutaneous transluminal angioplasty (PTA)
- Percutaneous transluminal coronary angioplasty (PTCA)
This guide wire may also be used with compatible stent devices.
This device is designed and intended for ONE-TIME USE ONLY. Do not resterilize and / or reuse.
CONTRAINDICATIONS
Not intended for use in the cerebral vasculature.
WARNINGS
Not intended for use with atherectomy devices.
Carefully observe the instructions under “Do Not” and “Do” below. Failure to do so may result in vessel trauma, guide wire damage, guide wire tip separation, or stent damage. If resistance is observed at any time, determine the cause under fluoroscopy and take remedial action as needed. Use the most suitable guide wire for the lesion being treated.
Do Not:
- Push, auger, withdraw, or torque a guide wire that meets resistance.
- Torque a guide wire if the tip becomes entrapped within the vasculature.
- Allow the guide wire tip to remain in a prolapsed condition.
- Deploy a stent such that it will entrap the wire between the vessel wall and the stent.
Do:
- Advance or withdraw the guide wire slowly.
- Use the radiopaque marker of the interventional device to confirm position.
- Examine the tip movement under fluoroscopy before manipulating, moving, or torquing the guide wire.
- Observe the wire under fluoroscopy for tip buckling, which is a sign of resistance.
- Maintain continuous flush while removing and reinserting the guide wire to prevent air from entering the catheter system. Perform exchanges slowly to prevent air entry and / or trauma.
- When reintroducing the guide wire, confirm that the interventional device tip is free within the vessel lumen and that the tip is parallel to the vessel wall.
- Use extreme caution when moving a guide wire through a non-endothelialized stent, or through stent struts, into a bifurcated vessel. Use of this technique involves additional patient risks, including the risk that the wire may become caught on the stent strut.
PRECAUTIONS
Guide wires are delicate instruments and should be handled carefully. Prior to use and when possible during the procedure, inspect the guide wire carefully for bends, kinks, or other damage. Do not use damaged guide wires. Using a damaged guide wire may result in vessel damage and / or inaccurate torque response.
Confirm the compatibility of the guide wire diameter with the interventional device before actual use.
Free movement of the guide wire within the interventional device is an important feature of a steerable guide wire system, because it gives the user valuable tactile information. Test the system for any resistance prior to use. Adjust or replace the hemostatic valve with an adjustable valve if it is found to inhibit guide wire movement.
Never attach the torque device to the modified portion of the proximal end of the extendible guide wire; otherwise, guide wire damage may occur, preventing the ability to attach the DOC™ Guide Wire Extension.
HI-TORQUE™ Guide Wires with Hydrophilic Coating: Avoid abrasion of the hydrophilic coating. Do not withdraw or manipulate the hydrophilic-coated wire through a metal cannula or sharp-edged object.
ADVERSE EVENTS
Potential adverse events associated with use of this device may include the following but not limited to perforation, dissection, occlusion, myocardial infarction, embolism and infection.
MAT-2104726 v2.0
HI-TORQUE TURNTRAC™
Guide Wire

INDICATIONS FOR USE
This HI-TORQUETM Guide Wire is intended to facilitate the delivery of catheter-based interventional devices during the following procedures:
• Percutaneous transluminal angioplasty (PTA)
• Percutaneous transluminal coronary angioplasty (PTCA)
This guide wire may also be used with compatible stent devices.
This device is designed and intended for ONE-TIME USE ONLY. Do not resterilize and / or reuse.
CONTRAINDICATIONS
Not intended for use in the cerebral vasculature.
WARNINGS
Not intended for use with atherectomy devices.
Carefully observe the instructions under “Do Not” and “Do” below. Failure to do so may result in vessel trauma, guide wire damage, guide wire tip separation, or stent damage. If resistance is observed at any time, determine the cause under fluoroscopy and take remedial action as needed. Use the most suitable guide wire for the lesion being treated.
Do Not:
- Push, auger, withdraw, or torque a guide wire that meets resistance.
- Torque a guide wire if the tip becomes entrapped within the vasculature.
- Allow the guide wire tip to remain in a prolapsed condition.
- Deploy a stent such that it will entrap the wire between the vessel wall and the stent.
Do:
- Advance or withdraw the guide wire slowly.
- Use the radiopaque marker of the interventional device to confirm position.
- Examine the tip movement under fluoroscopy before manipulating, moving, or torquing the guide wire.
- Observe the wire under fluoroscopy for tip buckling, which is a sign of resistance.
- Maintain continuous flush while removing and reinserting the guide wire to prevent air from entering the catheter system. Perform exchanges slowly to prevent air entry and / or trauma.
- When reintroducing the guide wire, confirm that the interventional device tip is free within the vessel lumen and that the tip is parallel to the vessel wall.
- Use extreme caution when moving a guide wire through a non-endothelialized stent, or through stent struts, into a bifurcated vessel. Use of this technique involves additional patient risks, including the risk that the wire may become caught on the stent strut.
PRECAUTIONS
Guide wires are delicate instruments and should be handled carefully. Prior to use and when possible during the procedure, inspect the guide wire carefully for bends, kinks, or other damage. Do not use damaged guide wires.
Using a damaged guide wire may result in vessel damage and / or inaccurate torque response.
This device should be used only by physicians trained in angiography and percutaneous transluminal coronary angioplasty (PTCA), and / or percutaneous transluminal angioplasty (PTA).
Confirm the compatibility of the guide wire diameter with the interventional device before actual use.
Free movement of the guide wire within the interventional device is an important feature of a steerable guide wire system, because it gives the user valuable tactile information. Test the system for any resistance prior to use. Adjust or replace the hemostatic valve with an adjustable valve if it is found to inhibit guide wire movement.
Never attach the torque device to the modified portion of the proximal end of the extendable guide wire; otherwise, guide wire damage may occur, preventing the ability to attach the DOCTM Guide Wire Extension.
HI-TORQUETM Guide Wires with Hydrophilic Coating: Avoid abrasion of the hydrophilic coating. Do not withdraw or manipulate the hydrophilic-coated wire through a metal cannula or sharp-edged object.
ADVERSE EVENTS
Potential adverse events associated with use ofthis device may include the following but not limited to:
- Perforation
- Dissection
- Occlusion
- Myocardial infarction
- Embolism
- Infection
- Allergic reaction or hypersensitivity to latex, contrast agent, anesthesia, device materials, and drug reactions to anticoagulation, or antiplatelet drugs
- Vasoconstriction
- Vasospasm
- Hypotension
- Hypertension
MAT-2104727 v2.0
HI-TORQUE PROGRESS™ Guide Wire, HI-TORQUE PILOT™ Guide Wire for PTCA, PTA, Stents, CTO

INDICATIONS FOR USE: Intended to facilitate the delivery of catheter-based interventional devices during percutaneous transluminal coronary angioplasty (PTCA) and percutaneous transluminal angioplasty (PTA). This guide wire may be used with compatible stent devices during therapeutic procedures. The guide wire may be used to reach and cross a target lesion, provide a pathway within the vessel structure, facilitate the substitution of one diagnostic or interventional device for another, and to distinguish the vasculature. This guide wire may also be used to cross or assist in crossing de novo chronic total coronary occlusions (CTO).
CONTRAINDICATIONS: Not intended for use in the cerebral vasculature or with atherectomy devices.
WARNINGS:
This device is designed and intended for ONE-TIME USE ONLY. Do not resterilize and / or reuse.
Carefully observe the instructions under “Do Not” and “Do” below. Failure to do so may result in vessel trauma, guide wire damage, guide wire tip separation, or stent damage. If resistance is observed at any time, determine the cause under fluoroscopy and take remedial action as needed. Use the most suitable guide wire for the lesion being treated.
Do Not:
- Push, auger, withdraw, or torque a guide wire that meets resistance.
- Torque a guide wire if the tip becomes entrapped within the vasculature.
- Allow the guide wire tip to remain in a prolapsed condition.
Do:
- Advance or withdraw the guide wire slowly.
- Use the radiopaque marker of the interventional device to confirm position.
- Examine the tip movement under fluoroscopy before manipulating, moving, or torquing the guide wire.
- Observe the wire under fluoroscopy for tip buckling, which is a sign of resistance.
- Maintain continuous flush while removing and reinserting the guide wire to prevent air from entering the catheter system. Perform exchanges slowly to prevent air entry and / or trauma.
- When reintroducing the guide wire, confirm that the interventional device tip is free within the vessel lumen and that the tip is parallel to the vessel wall.
- Use extreme caution when moving a guide wire through a non- endothelialized stent, or through stent struts, into a bifurcated vessel. Use of this technique involves additional patient risks, including the risk that the wire may become caught on the stent strut.
- Consider that if a secondary wire is placed in a bifurcation branch, this wire may need to be retracted prior to stent deployment, because there is additional risk that the secondary wire may become entrapped between the vessel wall and the stent.
For the HI-TORQUE PROGRESS™ family only: The HI- TORQUE PROGRESS™ family of guide wires has distal ends of varying stiffness. Operate these guide wires carefully so as to not injure the blood vessel, observing the information in these instructions. The higher torque performance, stiffer distal ends, and / or higher advancement force may present a higher risk of perforation or injury than a guide wire with a more pliable distal end. Therefore, use the guide wire with the least stiff distal end that will treat the lesion, and use extreme care to minimize the risk of perforation or other damage to blood vessels.
PRECAUTIONS
Guide wires are delicate instruments and should be handled carefully. Prior to use and when possible during the procedure, inspect the guide wire carefully for bends, kinks, or other damage. Do not use damaged guide wires. Using a damaged guide wire may result in vessel damage and / or inaccurate torque response.
Confirm the compatibility of the guide wire diameter with the interventional device before actual use.
Free movement of the guide wire within the interventional device is an important feature of a steerable guide wire system, because it gives the user valuable tactile information. Test the system for any resistance prior to use. Adjust or replace the hemostatic valve with an adjustable valve if it is found to inhibit guide wire movement.
Never attach the torque device to the modified portion of the proximal end of the extendible guide wire; otherwise, guide wire damage may occur, preventing the ability to attach the DOC™ Guide Wire Extension.
Avoid abrasion of the hydrophilic coating. Do not withdraw or manipulate the hydrophilic-coated wire through a metal cannula or sharp-edged object.
ADVERSE EVENTS
Potential Adverse Events associated with use of this device may include the following, but not limited to: perforation, dissection, occlusion, myocardial infarction, embolism and infection.
MAT-2213673 v1.0
HI-TORQUE™ Guide Wires

INTENDED USE
All HI-TORQUE™ Guide Wires are intended to facilitate the placement of balloon dilatation catheters during percutaneous transluminal coronary angioplasty (PTCA) and percutaneous transluminal angioplasty (PTA).
INDICATIONS
Refer to the device label for any additional product-specific indications that may apply.
CONTRAINDICATIONS
HI-TORQUE™ Guide Wires Wires are not intended for use in the cerebral vasculature. Refer to the device label for any additional product-specific contraindications that may apply.
WARNINGS
This device is designed and intended for ONE-TIME USE ONLY. Do not resterilize and / or reuse.
Carefully observe the instructions under “Do Not” and “Do” below. Failure to do so may result in vessel trauma, guide wire damage, guide wire tip separation, or stent damage. If resistance is observed at any time, determine the cause under fluoroscopy and take remedial action as needed. Use the most suitable guide wire for the lesion being treated.
Do Not:
- Push, auger, withdraw, or torque a guide wire that meets resistance.
- Torque a guide wire if the tip becomes entrapped within the vasculature.
- Allow the guide wire tip to remain in a prolapsed condition.
Do:
- Advance or withdraw the guide wire slowly.
- Use the radiopaque marker of the interventional device to confirm position.
- Examine the tip movement under fluoroscopy before manipulating, moving, or torquing the guide wire.
- Observe the wire under fluoroscopy for tip buckling, which is a sign of resistance.
- Maintain continuous flush while removing and reinserting the guide wire to prevent air from entering the catheter system. Perform exchanges slowly to prevent air entry and / or trauma.
- When reintroducing the guide wire, confirm that the interventional device tip is free within the vessel lumen and that the tip is parallel to the vessel wall.
- Use extreme caution when moving a guide wire through a non-endothelialized stent, or through stent struts, into a bifurcated vessel. Use of this technique involves additional patient risks, including the risk that the wire may become caught on the stent strut.
- Consider that if a secondary wire is placed in a bifurcation branch, this wire may need to be retracted prior to stent deployment because there is additional risk that the secondary wire may become entrapped between the vessel wall and the stent.
PRECAUTIONS
Guide wires are delicate instruments and should be handled carefully. Prior to use and when possible during the procedure, inspect the guide wire carefully for bends, kinks, or other damage. Do not use damaged guide wires. Using a damaged guide wire may result in vessel damage and / or inaccurate torque response.
Confirm the compatibility of the guide wire diameter with the interventional device before actual use.
Free movement of the guide wire within the interventional device is an important feature of a steerable guide wire system, because it gives the user valuable tactile information. Test the system for any resistance prior to use. Adjust or replace the hemostatic valve with an adjustable valve if it is found to inhibit guide wire movement.
Never attach the torque device to the modified portion of the proximal end of the extendable guide wire; otherwise, guide wire damage may occur, preventing the ability to attach the DOC™ Guide Wire Extension.
HI-TORQUE™ Guide Wires with Hydrophilic Coating: Avoid abrasion of the hydrophilic coating.
Do not withdraw or manipulate the hydrophilic-coated wire through a metal cannula or sharp-edged object.
ADVERSE EVENTS
Potential Adverse Events associated with use of this device may include the following but not limited to perforation, dissection, occlusion, myocardial infarction, embolism and infection.
MAT-2213672 v1.0
Teleport‡ MicroCatheter

Indications
The Teleport‡ microcatheters are indicated for:
- supporting and facilitating the placement of guidewires in the coronary and peripheral vasculature.
- exchanging guidewires in the coronary and peripheral vasculature.
- the delivery of contrast media into the coronary, peripheral, and abdominal vasculature.
Contraindications
The use of the Teleport‡ microcatheters are contraindicated:
- for use in patients with an unprotected left main coronary artery.
- for use in patients with arterial spasm in the absence of significant stenosis.
- for use in the neurovasculature.
Warnings
When using this type of device, the following warnings should be observed:
- This device is intended for single use only. Do not resterilize and/or reuse, as this can potentially result in compromised device performance and increased risk of crosscontamination.
- Do not modify this product for any reason. Modification of this product may compromise the integrity and performance of the product. Use of a modified product may result in vascular injury.
- The patient may suffer from subacute thrombosis, vascular complications, or bleeding complications by using this microcatheter. Therefore, it should be well examined if the intervention procedure will be applicable for the patient.
- The device must always be operated under high-resolution fluoroscopic guidance. Particular attention should be paid when inserting or withdrawing the device into stenotic areas, highly calcified lesions, stent struts, and narrower vessels than the product. Abrasion may result in damage or rupture of the device and the hydrophilic coating which may cause vascular injury, perforation, or distal emboli.
- If abnormal resistance is detected during use of this product, do not continue the operation, avoid excessive manipulations, and carefully remove the entire catheter system while paying full attention to avoid complications. Continuing the operation while the cause of the problem is not identified may cause damage to, or rupture of, the catheter, and damage the blood vessel.
- This microcatheter is coated with hydrophilic coating. Therefore, the microcatheter is highly lubricious. Always confirm the position of the distal end of the microcatheter by fluoroscopy and manipulate the microcatheter carefully.
- Do not insert the guidewire by force or advance it rapidly when the microcatheter is bent or twisted. Such manipulations may cause rupture or damage of the microcatheter, or perforation of the blood vessel.
- Always advance the guidewire ahead of the microcatheter before attempting any manipulation of the microcatheter. If the guidewire is not advanced ahead of the microcatheter, the blood vessel may be damaged or perforated, or the microcatheter may be damaged.
- Always hold the proximal hub with one hand and turn the catheter carefully while regularly releasing the accumulated torsion of the catheter. Never turn the catheter continuously while holding the proximal hub with both hands or use any other means to apply force. When releasing the accumulated torsion, be sure to open the hemostatic valve on the Y-connector. Do not turn the catheter in the same direction, either clockwise or counterclockwise, for more than 20 consecutive turns. If resistance is felt while turning the catheter, do not proceed with further rotation even if the 20-turn limit has not been reached. Identify the cause of resistance under fluoroscopy, and take appropriate action. Never continue the operation without identifying the cause; continuing rotation may damage or rupture the catheter or damage the blood vessel.
- When infusing contrast media, the device must be operated under high-resolution fluoroscopic guidance, confirming that the contrast media is being infused from the tip of the device. If the contrast media is not being infused, infusion must be stopped and the device must be replaced. If the device lumen is occluded, the device may be dilated, damaged, or ruptured, resulting in a life-threatening adverse event due to spurting contrast media.
- Injection pressure must not exceed 300 psi (the maximum injection pressure) when injecting contrast media using a power injector. Exceeding the maximum injection pressure may cause damage to the microcatheter.
- Discontinue injection if irregular resistance is felt at the syringe. The microcatheter may be bent or blocked. Excessive pressure may cause expansion and/or rupture of the microcatheter.
- Do not use a power injector to infuse contrast media when the microcatheter is bent or occluded. It may cause damage to the microcatheter such as expansion or breakage.
- Do not use guidewires larger than the recommended size. Resistance may be felt while advancing or withdrawing a guidewire larger than the recommended size, which may cause the catheter to become damaged or break, or the blood vessel to become damaged.
- If the device is inserted into vessels and the guidewire is to be replaced, insert the guidewire carefully. If any resistance is encountered, the operation must be discontinued immediately, and the device and the guidewire(s) withdrawn together. The device may be damaged and the tip may be cut.
- Do not wipe the surface of the microcatheter with gauze or absorbent cotton soaked with alcohols, gluconic acid chlorhexidine aqueous solution, or similar solutions as it may significantly deteriorate the lubricity of the microcatheter.
- Repeated insertion and withdrawal of the device may lead to deterioration of the hydrophilic coating. Continuous use of the device with deteriorated hydrophilic coating may cause vascular damage. This may also increase the risk of the tip being trapped, damaged, or ruptured.
Precautions
- Use the microcatheter prior to the "Use By" date specified on the package.
- Prior to use, the catheter should be examined to verify functionality and ensure that its size and length are suitable for the specific procedure for which it is to be used. Check to ensure that the microcatheter was not damaged during transportation. Do not use if the package and/or the product is suspected to be damaged.
- This product must be used under fluoroscopy by a physician who is fully trained in interventional procedures.
- Check the patient condition before the procedure. Provide appropriate anticoagulant therapy if necessary.
- When inserting the guidewire into the microcatheter that is already placed in the blood vessel, carefully operate the guidewire not to damage the microcatheter at the bend sections.
- When using a guiding catheter fitted with a stopcock, do not manipulate the stopcock after inserting the microcatheter into the guiding catheter. The microcatheter may be damaged if the stopcock is manipulated during the insertion.
- Operate the microcatheter carefully to avoid damage, kinks, or bends, especially when inserting into the guiding catheter.
- Flush the surface and the lumen of the microcatheter continuously with sterile heparinized saline during its use to maintain lubricity.
- When inserting or exchanging the microcatheter, flush the lumen of the guiding catheter and the microcatheter system continuously with sterile heparinized saline.
- This product is not intended for drug infusion other than contrast media. This product has not been designed for drug infusion other than contrast media and its safety has not been established for this indication.
- When infusing contrast media, read the Instructions for Use provided with such contrast media and comply with instructions, precautions, and warnings.
- Use the extension tube when contrast media is injected by using power injector.
- Confirm that the inserted microcatheter does not have a kink, knot, torsion, or occlusion before injecting contrast media.
- Flush the lumen of the microcatheter sufficiently with sterile heparinized saline especially after injecting contrast media.
- Discard all disposable devices used during this procedure per local requirements for medical device waste disposal.
Adverse Effects
Adverse events due to the use of this product include, but are not limited to, the following:
- Acute myocardial infarction
- Acute, or subacute, thrombosis
- Acute vessel closure
- Allergic reaction to device, contrast medium, or medication
- Aneurysm
- Arrhythmias
- Arteriovenous fistula
- Death
- Dissection (perforation, rupture, or injury) of the vessel
- Distal emboli
- Hemorrhage or hematoma
- Hypertension
- Hypotension
- Infection
- Ischemia
- Stroke by air embolism or embolization of fragments of thrombotic or atherosclerotic material
- Total occlusion of the artery resulting in ischemia
- Vascular spasm
CAUTION: This product is intended for use by or under the direction of a physician. Prior to use, reference the Instructions for Use, inside the product carton (when available), at manuals.eifu.abbott or at eifu.orbusneich.com for more detailed information on Indications, Contraindications, Warnings, Precautions and Adverse Events. This material is intended for use with healthcare professionals only.
MAT-2400961 v2.0
OPTIS™ and OPTIS™ Next Imaging Systems and Software

INDICATIONS
Applies to OPTIS™ Imaging Systems and Software
The OPTIS™ Software and AptiVue™ E Series Software are intended to be used only with compatible OPTIS™ Imaging Systems.
The OPTIS™ Imaging Systems with a compatible Dragonfly™ Imaging Catheter are intended for the imaging of coronary arteries and is indicated in patients who are candidates for transluminal interventional procedures. The compatible Dragonfly™ Imaging Catheters are intended for use in vessels 2.0 to 3.5 mm in diameter. The compatible Dragonfly™ Imaging Catheters are not intended for use in the left main coronary artery or in a target vessel which has undergone a previous bypass procedure.
The OPTIS™ Imaging Systems are intended for use in the catheterization and related cardiovascular specialty laboratories and will further compute and display various physiological parameters based on the output from one or more electrodes, transducers, or measuring devices. The physician may use the acquired physiological parameters, along with knowledge of patient history, medical expertise and clinical judgment to determine if therapeutic intervention is indicated.
Applies to OPTIS™ Next Imaging Systems and Software
The Ultreon™ 1.0 Software and Ultreon™ 2.0 Software are intended to be used only with compatible OPTIS™ Next Imaging Systems.
The OPTIS™ Next Imaging System with a compatible Dragonfly™ OPTIS™ Imaging Catheter or Dragonfly OpStar™ Imaging Catheter is intended for the imaging of coronary arteries and is indicated in patients who are candidates for transluminal interventional procedures. The Dragonfly™ OPTIS™ Imaging Catheter or Dragonfly OpStar™ Imaging Catheter is intended for use in vessels 2.0 to 3.5 mm in diameter. The Dragonfly™ OPTIS™ Imaging Catheter or Dragonfly OpStar™ Imaging Catheter is not intended for use in the left main coronary artery or in a target vessel which has undergone a previous bypass procedure.
The OPTIS™ Next Imaging Systems are intended for use in the catheterization and related cardiovascular specialty laboratories and will further compute and display various physiological parameters based on the output from one or more electrodes, transducers, or measuring devices. The physician may use the acquired physiological parameters, along with knowledge of patient history, medical expertise, and clinical judgment to determine if therapeutic intervention is indicated.
Applies to both OPTIS™ and OPTIS™ Next Imaging Systems and Software
The Dragonfly™ OPTIS™ or Dragonfly™ OpStar™ Imaging Catheters are intended for use in vessels 2.0 to 3.5 mm in diameter. The Dragonfly™ OPTIS™ or Dragonfly™ OpStar™ Imaging Catheters are not intended for use in the left main coronary artery or in a target vessel which has undergone a previous bypass procedure.
The OPTIS™ and OPTIS™ Next Imaging Systems are intended for use in the catheterization and related cardiovascular specialty laboratories and will further compute and display various physiological parameters based on the output from one or more electrodes, transducers, or measuring devices. The physician may use the acquired physiological parameters, along with knowledge of patient history, medical expertise, and clinical judgment to determine if therapeutic intervention is indicated.
CONTRAINDICATIONS
The OPTIS™ and OPTIS™ Next Integrated Systems and Mobile Systems with the usage of the OPTIS™ Software, AptiVue™ E Series Software, Ultreon™ 1.0 Software, and Ultreon™ 2.0 Software are contraindicated where introduction of any catheter would constitute a threat to patient safety. Contraindications include:
- Bacteremia or sepsis
- Major coagulation system abnormalities
- Patients diagnosed with coronary artery spasm
- Patients disqualified for coronary artery bypass graft (CABG) surgery
- Patients disqualified for percutaneous transluminal coronary angioplasty (PTCA)
- Severe hemodynamic instability or shock
- Total occlusion
- Large thrombus
- Acute renal failure
- Inability to tolerate systemic anticoagulation is a contraindication to use of OCT for coronary imaging.
- The system has no patient alarm functions. Do not use for cardiac monitoring.
COMPLICATIONS
The following complications may occur as a consequence of intravascular imaging and catheterization procedure:
- Abnormal heart rhythm or arrhythmias
- Acute myocardial infarction
- Allergic reaction to the contrast media or drug administered for the procedure
- Arterial dissection, injury, or perforation
- Bleeding
- Catheter access site reactions: inflammation or granuloma
- Coronary artery spasm
- Death
- Embolism
- Hypotension
- Infection
- Myocardial ischemia
- Renal insufficiency or failure from contrast media use
- Repeat revascularization
- Thrombus formation, abrupt closure, or total occlusion
- Tissue necrosis
- Unstable angina
WARNINGS
- Prior to use, please review the Instructions for Use supplied with the OPTIS™ imaging system, Dragonfly™ Imaging Catheter, Wi-Box™ AO Transmitter and the PressureWire™ guidewire for more information.
- The Dragonfly™ Imaging Catheter is sterilized by ethylene oxide and is intended for one time use only. Non-pyrogenic. Do not use if the package is opened or damaged. Do not reuse or re-sterilize. Any attempt to reuse or re-sterilize may compromise the structural integrity of this device. Adverse effects of using a non-sterile or re-sterilized catheter may include, but are not limited to: local and / or systemic infection, mechanical damage, inaccurate results.
- Appropriate anticoagulant and vasodilator therapy must be used during the procedure as needed.
- Ensure that no air is introduced into the system during the Dragonfly™ Imaging Catheters insertion.
- Observe all advancement and movement of the Dragonfly™ Imaging Catheters under fluoroscopy. Always advance and withdraw the catheter slowly. Failure to observe device movement fluoroscopically may result in vessel injury or device damage. To ensure proper placement, do not move the guide wire after a Dragonfly™ Imaging Catheter is in place.
- If resistance is encountered during advancement or withdrawal of the Dragonfly™ Imaging Catheter, stop manipulation and evaluate under fluoroscopy. If the cause of resistance cannot be determined or mitigated, carefully remove the Dragonfly™ Imaging Catheters and guidewire together as a unit from the patient.
- Leave the guide wire engaged with a Dragonfly™ Imaging Catheter at all times during use. Do not withdraw or advance the guide wire prior to withdrawing the Dragonfly™ Imaging Catheters.
- The Dragonfly™ Imaging Catheters should never be forced into lumens that are narrower than the Dragonfly™ Imaging Catheters body or forced through a tight or heavily calcified lesion.
- The Dragonfly™ Imaging Catheters should not be advanced through abnormally tortuous anatomy.
- When advancing or retracting a Dragonfly™ Imaging Catheter with a monorail tip through a stented vessel, the Dragonfly™ Imaging Catheters may engage the stent between the junction of the Dragonfly™ Imaging Catheters and guide wire, resulting in entrapment of catheter / guide wire, catheter tip separation, stent dislocation, and / or vascular injury.
- Refer to the contrast media Instructions for Use for general warnings and precautions relating to use of contrast media.
- Before creating an OCT recording, review “Performing an OCT Procedure” for additional warnings and cautions in the IFU.
PRECAUTIONS
- Safety and effectiveness have been established for the following patient population: adult patients undergoing non-emergent percutaneous coronary interventions in lesions with reference vessel diameters between 2.0 to 3.5 mm, which are not located in the left main coronary artery or in a target vessel which has undergone previous bypass procedures.
- Follow all instructions, warnings, and cautions provided in “Patient Safety” in the IFU.
- All operators must be knowledgeable in performing OCT and physiological procedures prior to using the OPTIS™ and OPTIS™ Next Integrated Systems and Mobile Systems with the usage of the OPTIS™ Software, AptiVue™ E Series Software, Ultreon™ 1.0 Software, and Ultreon™ 2.0 Software.
- When using saline, heparinized saline is recommended.
- Monitor the OCT image for indications of the Dragonfly™ Imaging Catheters optical failure. If optical failure is suspected, remove the Dragonfly™ Imaging Catheter from the patient, press “Unload” on the drive motor and optical controller (DOC), detach the catheter, and replace it with a new one.
- If the pullback triggers before contrast is injected, repeat the pullback.
- For optimal imaging, only use 100% contrast media.
- Use the minimum flush rate and volume required to image the desired anatomy.
- To obtain accurate measurements, be sure the selection for the Flush Medium is the same as the medium in which you are imaging.
- The Dragonfly™ Imaging Catheters must be purged prior to connection to the DOC to prevent damage to the imaging core.
- Do not insert or remove a Dragonfly™ Imaging Catheter while the DOC is scanning. Do not attempt to disconnect the catheter from the DOC while the “lock” LED is blinking as it could damage the catheter or the DOC. Refer to “Removing the Dragonfly™ Imaging Catheter” in the IFU.
- Never attempt to attach or detach a catheter to the DOC while the "lock" LED is lit.
- Take care in handling the Dragonfly™ Imaging Catheters to prevent breaking the fiber-optics within the catheter. Kinking and bending of the catheter can cause damage. While connecting, ensure the proximal catheter segment is straight and aligned with the DOC. Never attempt to connect and operate the catheter while the catheter remains coiled within the hoop.
- Do not kink, sharply bend, pinch, or crush the Dragonfly™ Imaging Catheters at any time.
- The Dragonfly™ Imaging Catheters have no user serviceable parts. Do not attempt to repair or alter any part of the catheter assembly as provided.
- If you want to make measurements on files that will be exported to standard formats, you must make the measurements BEFORE exporting the images. Using non-OCT software to measure standard format images will not produce accurate measurements.
- Do not use images that have been exported to JPEG or Compressed AVI formats for clinical decision making. These formats use compression methods that may degrade the image quality.
- Artifacts may result in misrepresentation of L-mode data, so L-mode is not recommended for quantification of clinical information.
- It is the user’s responsibility to confirm the lumen contours of all the frames within the reference segment, and to make adjustments if necessary. Red frames indicate low confidence in the detected contours.
- Deleted files cannot be restored. After files have been deleted, they can only be imported back to your system from your archived copies.
- Restoring factory default settings resets ALL user-entered configuration values except the date and time. This button should be used only under the direction of qualified service personnel.
MAT-2309288 v1.0
Dragonfly OpStar™ Imaging Catheter

Indications: The Dragonfly OpStar™ Imaging Catheter with the OCT Imaging System is intended for the imaging of coronary arteries and is indicated in patients who are candidates for transluminal interventional procedures. The Dragonfly OpStar™ Imaging Catheter is intended for use in vessels 2.0 to 3.5 mm in diameter. The Dragonfly OpStar™ Imaging Catheter is not intended for use in the left main coronary artery or in a target vessel which has undergone a previous bypass procedure.
Contraindications: Use of the Dragonfly OpStar™ Imaging Catheter is contraindicated where introduction of any catheter would constitute a threat to patient safety. Contraindications include:
- Acute renal failure
- Bacteremia or sepsis
- Large thrombus
- Major coagulation system abnormalities
- Patients diagnosed with coronary artery spasm
- Patients disqualified for coronary artery bypass graft (CABG) surgery
- Patients disqualified for percutaneous transluminal coronary angioplasty (PTCA)
- Severe hemodynamic instability or shock
- Total occlusion
- Inability to tolerate systemic anticoagulation is a contraindication to use of OCT for coronary imaging
Warnings:
- Appropriate anticoagulant and vasodilator therapy is recommended to be used during the procedure as ordered by the physician.
- The Dragonfly OpStar™ Imaging Catheter is sterilized by ethylene oxide and is intended for one time use only. Nonpyrogenic. Do not use if the package is opened or damaged. Do not reuse or re-sterilize. Any attempt to reuse or re-sterilize may compromise the structural integrity of this device. Adverse effects of using a non-sterile or re-sterilized imaging catheter may include, but are not limited to:
- Local and/or systemic infection
- Mechanical damage
- Inaccurate results
- Note the product "Use by" date on the package.
- Observe all advancement and movement of the Dragonfly OpStar™ Imaging Catheter under fluoroscopy. Always advance and withdraw the catheter slowly and ensure that the guide wire is coaxial to the monorail. Failure to observe device movement fluoroscopically may result in vessel injury or device damage. To ensure proper placement, do not move the guide wire after the Dragonfly OpStar™ Imaging Catheter is in place.
- If resistance is encountered during withdrawal of the Dragonfly OpStar™ Imaging Catheter:
- Stop manipulation and evaluate under fluoroscopy.
- If guide wire prolapse is observed, readvance the catheter, ensure the guide wire is coaxial - to the monorail, and reattempt withdrawal.
- If the cause of resistance cannot be determined or mitigated, carefully remove the Dragonfly OpStar™ Imaging Catheter and guide wire as a unit from the patient and replace the Dragonfly OpStar™ Imaging Catheter and guide wire. Do not reuse the Dragonfly OpStar™ Imaging Catheter and guide wire.
- Leave the guide wire engaged with the Dragonfly OpStar™ Imaging Catheter at all times during use. Do not retract or advance the guide wire prior to withdrawing the Dragonfly OpStar™ Imaging Catheter.
- The Dragonfly OpStar™ Imaging Catheter should never be forced into lumens that are narrower than the catheter body or forced through a tight or heavily calcified lesion.
- The Dragonfly OpStar™ Imaging Catheter should not be advanced through abnormally tortuous anatomy.
- When advancing or retracting a Dragonfly OpStar™ Imaging Catheter with a monorail tip through a stented vessel, the Dragonfly imaging catheter may engage the stent between the junction of the Dragonfly OpStar™ Imaging Catheter and guide wire, resulting in entrapment of the catheter/guide wire, catheter tip separation, stent dislocation and/or vascular injury.
- Do not remove the Dragonfly OpStar™ Imaging Catheter from the DOC until the procedure is complete to avoid a potential sterility breach.
- Always verify that the Dragonfly OpStar™ Imaging Catheter has been properly prepared prior to inserting into vasculature.
- The safety and effectiveness of the coated device has not been established, or is unknown, in vascular regions other than those specifically indicated.
- Failure to abide by the warnings in this Instructions for Use might result in damage to the device coating, which may necessitate intervention or result in serious adverse events.
Precautions:
- Safety and effectiveness have been established for the following patient population: adult patients undergoing non-emergent percutaneous coronary interventions in lesions with reference vessel diameters between 2.0 mm to 3.5 mm, which were not located in the left main coronary artery or in a target vessel which has undergone a previous bypass procedure.
- Use the minimum flush rate and volume required to image the desired anatomy.
- For optimal imaging, only use 100% contrast media.
- Refer to contrast media Instructions for Use for general warnings and precautions relating to contrast media.
- Do not kink, sharply bend, pinch, or crush the Dragonfly OpStar™ Imaging Catheter at any time.
- The Dragonfly OpStar™ Imaging Catheter has no user serviceable parts. Do not attempt to repair or alter any part of the Dragonfly OpStar™ Imaging Catheter assembly as provided.
- After use, the Dragonfly OpStar™ Imaging Catheter may be a potential biohazard. Handle and dispose of in accordance with accepted medical practice and applicable laws and regulations.
- When using saline, heparinized saline is recommended. When wet, the hydrophilic coating increases the lubricity of the coated surface.
- Avoid abrasion of the hydrophilic coating. Use caution when manipulating, advancing and / or withdrawing these devices through needles, metal cannulas, stents, or other devices with sharp edges, or through tortuous or calcified blood vessels. Manipulation, advancement, and / or withdrawal past sharp or beveled edges may result in destruction and / or separation of the outer coating, which may lead to clinical adverse events, resulting in coating material remaining in the vasculature or device damage. This may result in adverse events requiring additional intervention.
- The integrity and performance of the device coating can be negatively impacted by preparation with incompatible media or solvents. Please take note of the following important recommendations:
- Avoid wiping the device with dry gauze as this may damage the device coating.
- Avoid excessive wiping of the coated device.
- Avoid using alcohol, antiseptic solutions, or other solvents to pre-treat the device because this may cause unpredictable changes in the coating which could negatively affect the safety and performance of the catheter.
- Do not soak the device as it may adversely impact the hydrophilic coating on the catheter.
- The Dragonfly OpStar™ Imaging Catheter must be purged prior to connection to the DOC to prevent damage to the imaging core.
- Ensure that the Dragonfly OpStar™ Imaging Catheter tip marker has been properly identified and differentiated from the lens marker before contrast administration and prior to performing the OCT reading.
- Never attempt to attach or detach the Dragonfly OpStar™ Imaging Catheter to the DOC while the "lock" LED is lit.
Complications:
The following complications may occur as a consequence of intravascular imaging and catheterization procedure:
- Allergic reaction to the contrast media or drug administered for the procedure
- Bleeding
- Arterial dissection, injury or perforation
- Abnormal heart rhythm or arrhythmias
- Unstable angina
- Coronary artery spasm
- Thrombus formation, abrupt closure, or total occlusion
- Embolism
- Infection
- Myocardial ischemia
- Acute myocardial infarction
- Repeat revascularization
- Renal insufficiency or failure from contrast media use
- Death
- Catheter access side reactions: inflammation or granuloma or tissue necrosis
- Hypotension
MAT-2115499 v3.0
Coroventis‡ CoroFlow‡ Cardiovascular System

Indications: CoroFlow‡ is indicated to provide hemodynamic information for use in the diagnosis of patients with cardiovascular diseases.
CoroFlow‡ is intended for use in catheterization and related cardiovascular specialty laboratories to compute and display various physiological parameters based on the output from one or more measuring devices.
Contraindications: The system has no patient alarm functions. Do not use for cardiac/vital signs monitoring.
Warnings:
- If CoroFlow‡ is used together with 3rd party infusion catheters for assessment of Absolute Flow and Resistance, ensure that the maximum infusion rate per manufacturers instruction is not exceeded or vessel injury may occur.
- Do not use the CoroFlow‡ Cardiovascular System if there is reason to believe the system's security has been compromised or if the system was unaccounted for a period of time (i.e. misappropriated, modified or tampered with).
- Do not leave the CoroFlow‡ Cardiovascular System unattended when logged in as a PC Administrator.
- To protect the privacy and security of sensitive information, including electronic protected health information (EPHI), and to protect the integrity of the system itself, the system should be located in a physically secure, access-controlled environment.
- To protect the privacy and security of sensitive information, including electronic protected health information (EPHI), the PC on to which CoroFlow‡ is installed must be configured according to the Installation Instructions in this manual. Failure to configure the PC correctly may result in increased risk for unauthorized release of protected health information. Windows settings include:
- Activation and configuration of restricted user Access
- Activation of Windows Firewall and blocking of network connections
- Activation of Windows Bitlocker drive encryption
- Activation of Windows Secure Boot
- Activation of Windows Anti-Virus scanning and ransomware protection. Ensure CoroFlow‡ is added in the list of trusted applications.
- Activation of Windows update
- Disable unused interfaces
- Use of this equipment adjacent to or stacked with other equipment should be avoided because it could result in improper operation. If such use is necessary, this equipment and the other equipment should be observed to verify that they are operating normally.
- Use of accessories, transducers and cables other than those specified or provided by Coroventis‡ could result in increased electromagnetic emissions or decreased electromagnetic immunity of this equipment and result in improper operation.
- Portable RF communications equipment (including peripherals such as antenna cables and external antennas) should be used no closer than 30 cm (12 inches) to any part of CoroFlow‡, including cables specified by Coroventis‡. Otherwise, degradation of the performance of this equipment could result.
Precautions:
- The PC and CoroHub‡ shall not be placed within the patient environment (1.5 m from patient).
- For operation of other devices used in conjunction with CoroFlow‡ consult the IFU for each of these devices for details on indication, handling and safety information.
- It is recommended to ensure local routines for data backup of stored recordings. CoroFlow‡ does not create backup of stored data.
- Always check minimum performance requirement on PC to ensure compatibility with CoroFlow‡.
- It is recommended to install CoroFlow‡ on a PC with backup battery to avoid interruption in case of power failure.
- Always manually review and confirm valid cursor positions and detected heart beats.
- Ensure that Pa and Pd pressure waveforms are aligned in phase and offset after equalization, or indices can be mis-calculated.
- Confirm that the correct Wi-Box is selected by manually matching the Wi-Box ID number with the Wi-Box in the lab.
- Changing parameter settings outside of default values may affect measurement performance, only for research purposes.
- Only to be used by healthcare professionals.
- Using a network location to store data may cause previously unidentified risks if the network malfunctions.
- No modification or tampering with CoroFlow‡ is permitted.
- CoroFlow‡, including accessories and components, shall not be used if it has been subject to damage.
- The assembly of medical electrical systems and modifications during the actual service life require evaluation to the requirements according to IEC 60601-1 standard series.
- CoroHub‡ does not have any serviceable parts and require no field maintenance. No modification or tampering with CoroHub‡ is permitted.
- CoroHub‡ shall not be immersed in liquid.
- CoroHub‡ shall not be used if it has been subject to damage.
- PPG values may be non-unique and different combinations or focal/diffuse disease may result in the same PPG value.
- Direct connection to a non-secure network, like the internet, may interfere with correct operation and/or result in inappropriate access to patient information. Furthermore, it should be noted that reconfiguring a used network may lead to inability to import patient as well as export examination data, ultimately leading to a risk of loss of patient and examination data. To avoid this problem Coroventis‡ recommends verifying network settings in the system setup after each change. The same caution is relevant regarding connection to DICOM.
- Always confirm valid pressure tracings, marker positions and selected beats.
- Resetting CoroHub‡ will reset PressureWire connections and Zeroing/Equalization parameters.
MAT-2007904 v4.0
PressureWire™ X Guidewire

Indications: The PressureWire™ X Guidewire is indicated to direct a catheter through a blood vessel and to measure physiological parameters in the heart and in the coronary and peripheral blood vessels. Physiological parameters include blood pressure. The PressureWire™ X Guidewire can also measure blood temperature.
Contraindications: This guidewire is contraindicated for use in the cerebral vasculature.
Warnings:
- No modification of this device is allowed.
- The PressureWire™ X Guidewire is supplied sterile. Discard the guidewire if the pouch is opened or damaged, compromising the sterile barrier. The guidewire is designed for single use only and shall not be reused or resterilized. Adverse effects of using a non-sterile or resterilized guidewire may include, but are not limited to:
- Local and/or systemic infection
- Mechanical damage
- Inaccurate readings
- Observe all guidewire movements. Whenever the guidewire is moved or torqued, the tip movement should be examined under fluoroscopy. Never push, withdraw, or torque the guidewire if it meets resistance or without observing corresponding movement of the tip, otherwise vessel/ventricle trauma may occur.
- Torquing or excessive manipulation of the guidewire in a sharp bend, against resistance, or repeated attempts to cross a total vessel occlusion may:
- Cause dissection or perforation of blood vessels
- Cause vessel spasm
- Damage and/or fracture the guidewire
- When introducing the guidewire, flush the catheter and administer anticoagulation as for a standard catheterization procedure or clotting may occur.
- Do not use the guidewire in the ventricles if the patient has a prosthetic mechanical or biological valve. It may result in damage to both the prosthesis and the guidewire, which may cause injury or death.
- Use of the PressureWire™ X Guidewire in conjunction with interventional devices with a short rapid exchange may result in a folded or fractured guidewire.
- High frequency surgical devices must not be used on a patient at the same time as the guidewire.
Precautions:
- The PressureWire™ X Guidewire is a delicate instrument and should be handled carefully.
- Make sure that the transmitter is kept dry to ensure accurate pressure and/or temperature readings. Inaccurate readings may necessitate device replacement.
- Do not use the guidewire in conjunction with atherectomy catheters. It may damage the guidewire.
- Do not withdraw or manipulate the guidewire in a sharp-edged object. It may result in abrasion of the guidewire coating.
- Factors that may affect the accuracy of the diagnostic information include, but are not limited to:
- Improper placement of the aortic pressure sensor.
- Failure to achieve maximum coronary and myocardial hyperemia in FFR procedures.
- Blood flow affected by the position of interventional devices, such as balloon catheters.
- Guidewire readings may be affected by defibrillation. Rezero the guidewire after defibrillation use.
- Do not measure pressure when the guidewire sensor element is in a sharp bend or in contact with atrial or ventricular walls. It might result in pressure artifacts.
- Do not use the PressureWire™ X Guidewire together with another guidewire, for so called jailed wire technique, due to difficulty in guidewire withdrawal and possible guidewire entrapment.
- Store at room temperature (15°C – 25°C) in a dry and dark place.
Potential Adverse Events: Potential complications which may be encountered during all catheterization procedures include, but are not limited to: vessel dissection or occlusion, perforation, embolus, spasm, local and/or systemic infection, pneumothorax, congestive heart failure, myocardial infarction, hypotension, chest pain, renal insufficiency, serious arrhythmias, or death.
In addition, this device has a coating containing Polyethylene Glycol (PEG); potential allergic reactions (anaphylaxis) may occur during the interventional procedure if the patient is allergic to PEG.
MAT-2103599 v2.0
NC TREK NEO™
Coronary Dilatation Catheter

Indications For Use
The NC TREK NEO™ Coronary Dilatation Catheters are indicated for:
a) balloon dilatation of the stenotic portion of a coronary artery or bypass graft stenosis, for the purpose of improving myocardial perfusion
b) balloon dilatation of a coronary artery occlusion, for the purpose of restoring coronary flow in patients with ST-segment elevation myocardial infarction
c) balloon dilatation of a stent after implantation (balloon models 2.00 mm – 5.00 mm only)
Contraindications
The NC TREK NEO™ Coronary Dilatation Catheter is contraindicated for treatment of the unprotected left main coronary artery and for coronary artery spasm in the absence of a significant stenosis
Warnings
This device is intended for one time use only. DO NOT resterilize and / or reuse it, as this can compromise device performance and increase the risk of cross contamination due to inappropriate reprocessing.
Note the “Use by” date specified on the package.
The outside diameter (OD) of the distal 38 cm of the device, including the distal shaft, tip, and the balloon are coated with HYDROCOAT™ Hydrophilic Coating. Refer to PREPARATIONS FOR USE section of these instructions for further information on how to prepare and use this device to ensure it performs as intended. Failure to abide by the warnings in this labeling might result in damage to the device coating, which may necessitate intervention or result in serious adverse events.
Percutaneous transluminal coronary angioplasty (PTCA) should only be performed at centers where emergency coronary artery bypass graft surgery is available.
PTCA in patients who are not acceptable candidates for coronary artery bypass graft surgery requires careful consideration, including possible hemodynamic support during PTCA, as treatment of this patient population carries special risk.
Persons with known history of allergies to any of the components of this device listed below may suffer an allergic reaction to this coronary dilatation catheter. Prior to its use on the patient, the patient should be counseled on the materials contained in the device, and a thorough history of allergies must be discussed. This device contains: polyethylene oxide coating, polyamide, polyether block amide (PEBAX), polyethylene and stainless steel.
Use only the appropriate balloon inflation media. Do not use air or any gaseous medium to inflate the balloon. If gaseous medium is used and balloon rupture occurs there is a potential of causing air embolism and / or vessel injury. Balloon pressure should not exceed the rated burst pressure (RBP). Use of a pressure-monitoring device is recommended to prevent over pressurization.
To reduce the potential for vessel damage, the inflated diameter of the balloon should approximate the diameter of the normal or undiseased vessel segment, just proximal and distal to the stenosis.
Do not use or attempt to straighten a catheter if the shaft has become bent or kinked; this may result in the shaft breaking. Instead, prepare a new catheter.
Treatment of moderately or heavily calcified lesions is considered to be moderate risk, with increase in the risk of acute closure, vessel trauma, balloon burst, balloon entrapment, and associated complications. If resistance is felt, determine the cause before proceeding.
Continuing to advance or retract the catheter while under resistance may result in damage to the vessels and / or damage / separation of the catheter.
Precautions
When the catheter is exposed to the vascular system, it should be manipulated while under high quality fluoroscopic observation. Do not advance or retract the catheter unless the balloon is fully deflated under vacuum. If resistance is met during manipulation, determine the cause of the resistance before proceeding.
Do not torque the catheter more than one (1) full turn.
In the event of catheter damage / separation, retrieval methods (use of additional wires, snares, and / or forceps) may result in additional trauma to the coronary vasculature and / or the vascular access site. Complications may include bleeding, hematoma, or pseudoaneurysm.
To confirm sterility has been maintained, ensure that the package sterile barrier has not been opened or damaged prior to use. Inspect all product and ensure that the device is not damaged. Care must be taken to properly size the balloon prior to use.
During the procedure, appropriate anticoagulant and coronary vasodilator therapy must be provided to the patient as needed. Anticoagulant therapy should be continued for a period of time as determined by the physician after the procedure.
If the surface of the coronary dilatation catheter becomes dry, wet with heparinized normal saline to reactivate the coating.
Do not reinsert the coronary dilatation catheter into the coil dispenser after procedural use
The safety and effectiveness of these devices have not been established, or is unknown, in vascular regions other than those specifically indicated:
- PTCA balloon catheter for the treatment of in-stent restenosis (ISR) has not been established.
- The pediatric population.
- Balloon sizes 1.5 mm, 5.5 mm and 6.0 mm have not been established for balloon dilatation of a stent after implantation.
Potential Adverse Events
Possible adverse effects include, but are not limited to, the following:
- Allergic reaction or hypersensitivity to latex, contrast agent, anesthesia, device materials, and drug reactions to anticoagulation, or antiplatelet drugs
- Vascular access complications which may require transfusion or vessel repair including: Catheter site reactions, Bleeding (ecchymosis, oozing, hematoma, hemorrhage, retroperitoneal hemorrhage), Arteriovenous fistula, pseudoaneurysm, aneurysm, dissection, perforation /rupture, Embolism (air, tissue, plaque, thrombotic material, or device), Peripheral nerve injury, Peripheral ischemia
- Coronary artery or bypass graft complications which may require additional intervention, including:Total occlusion or abrupt closure, Arteriovenous fistula, pseudoaneurysm, aneurysm, dissection, perforation /rupture, Embolism (air, tissue, plaque, thrombotic material, or device), Thrombosis, Stenosis or restenosis
- Pericardial complication which may require additional intervention such as cardiac tamponade, pericardial effusion
- Cardiac arrhythmias (including conduction disorders, atrial and ventricular arrhythmias)
- Cardiac ischemic conditions (including myocardial ischemia, myocardial infarction [including acute], coronary artery spasm and unstable or stable angina pectoris)
- Stroke / cerebrovascular accident (CVA) and transient ischemic attack (TIA)
- System organ failures: Cardio-respiratory arrest, Cardiac failure, Cardiopulmonary failure (including pulmonary edema), Renal insufficiency
- Blood cell disorders (including heparin induced thrombocytopenia)
- Hypertension / hypotension
- Infection
- Nausea and vomiting
- Palpitation, dizziness, and syncope
- Chest pain
- Fever
- Pain
- Death
MAT-2206959 v3.0
TREK™ RX & OTW and MINI TREK™ RX & MINI TREK™ II OTW
Coronary Dilatation Catheters

Caution
CAREFULLY READ ALL INSTRUCTIONS PRIOR TO USE. OBSERVE ALL WARNINGS AND PRECAUTIONS NOTED THROUGHOUT THESE INSTRUCTIONS. FAILURE TO DO SO MAY RESULT IN COMPLICATIONS.
Indications
Applies to TREK™ RX & OTW 2.25 mm – 5.00 mm sizes only:
The TREK™ RX & OTW Coronary Dilatation Catheters are indicated for:
- Balloon dilatation of the stenotic portion of a coronary artery or bypass graft stenosis, for the purpose of improving myocardial perfusion
- Balloon dilatation of a coronary artery occlusion, for the purpose of restoring coronary flow in patients with ST-segment elevation myocardial infarction
- Balloon dilatation of a stent after implantation
Applies to MINI TREK™ RX and MINI TREK™ II OTW
1.50 mm – 2.00 mm sizes only:
The TREK™ RX & OTW Coronary Dilatation Catheters are indicated for:
- Balloon dilatation of the stenotic portion of a coronary artery or bypass graft stenosis, for the purpose of improving myocardial perfusion
- Balloon dilatation of a coronary artery occlusion, for the purpose of restoring coronary flow in patients with ST-segment elevation myocardial infarction
- Balloon dilatation of a stent after implantation (balloon model 2.0 mm only)
- Balloon dilatation of de novo chronic total coronary occlusions (CTO)
Applies to MINI TREK™ RX and MINI TREK™ II OTW 1.20 mm sizes only:
The MINI TREK™ RX and MINI TREK™ II OTW 1.20mm Coronary Dilatation Catheters are indicated for:
- Initial balloon dilatation of the stenotic portion of a coronary artery or bypass graft stenosis (≥ 70% stenosis).
- Balloon dilatation of de novo chronic total coronary occlusions (CTO)
Note (applies to 2.00 mm to 5.00 mm only): Post-deployment stent expansion testing was performed on the bench with the MULTI-LINK VISION™ and MULTI-LINK ULTRA™ stents. All stents should be deployed in accordance with the manufacturer’s indications and instructions for use.
Contraindications (applies to all sizes)
The TREK™ RX & OTW, MINI TREK™ RX and MINI TREK™ II OTW Coronary Dilatation Catheters are not intended to be used to treat patients with:
- An unprotected left main coronary artery
- A coronary artery spasm in the absence of a significant stenosis
Warnings (applies to all sizes)
This device is intended for one time use only. DO NOT resterilize and / or reuse it, as this can compromise device performance and increase the risk of cross contamination due to inappropriate reprocessing.
Percutaneous transluminal coronary angioplasty (PTCA) should only be performed at hospitals where emergency coronary artery bypass graft surgery can bequickly performed in the event of a potentially injurious or life-threatening complication.
PTCA in patients who are not acceptable candidates for coronary artery bypass graft surgery requires careful consideration, including possible hemodynamic support during PTCA, as treatment of this patient population carries special risk.
Use only the recommended balloon inflation medium. Never use air or any gaseous medium to inflate the balloon.
Balloon pressure should not exceed the rated burst pressure (RBP). The RBP is based on results of in vitro testing. At least 99.9% of the balloons (with a 95% confidence) will not burst at or below their RBP. Use of a pressure-monitoring device is recommended to prevent overpressurization.
To reduce the potential for vessel damage, the inflated diameter of the balloon should approximate the diameter of the vessel just proximal and distal to the stenosis.
When the catheter is exposed to the vascular system, it should be manipulated while under high quality fluoroscopic observation. Do not advance or retract the catheter unless the balloon is fully deflated under vacuum. If resistance is met during manipulation, determine the cause of the resistance before proceeding.
Do not use, or attempt to straighten, a catheter if the shaft has become bent or kinked; this may result in the shaft breaking. Instead, prepare a new catheter.
Do not torque the catheter more than one (1) full turn.
Treatment of moderately or heavily calcified lesions is considered to be moderate risk, with an expected success rate of 60 – 85% and increases the risk of acute closure, vessel trauma, balloon burst, balloon entrapment, and associated complications. If resistance is felt, determine the cause before proceeding. Continuing to advance or retract the catheter while under resistance may result in damage to the vessels and / or damage / separation of the catheter.
In the event of catheter damage / separation, recovery of any portion should be performed based on physician determination of individual patient condition and appropriate retrieval protocol.
Precautions (applies to all sizes)
Note the “Use by” date specified on the package.
Inspect all product prior to use. Do not use if the package is open or damaged.
This device should be used only by physicians trained in angiography and PTCA, and / or percutaneous transluminal angioplasty (PTA).
Prior to angioplasty, the dilatation catheter should be examined to verify functionality and ensure that its size is suitable for the specific procedure for which it is to be used.
During the procedure, appropriate anticoagulant and coronary vasodilator therapy must be provided to the patient as needed. Anticoagulant therapy should be continued for a period of time to be determined by the physician after the procedure.
If the surface of the TREK™ RX & OTW, MINI TREK™ RX or MINI TREK™ II OTW Coronary Dilatation Catheter becomes dry, wetting with heparinized normal saline will reactivate the coating.
Do not reinsert the TREK™ RX & OTW, MINI TREK™ RX or MINI TREK™ II OTW Coronary Dilatation Catheter into the coil dispenser after procedural use.
The safety and effectiveness of this PTCA balloon catheter for the treatment of in-stent restenosis (ISR) have not been established.
Applies to TREK™ RX and MINI TREK™ RX only (APPLIES TO ALL SIZES), in addition to above:
The design and construction of these catheters do not provide the user with distal pressure monitoring capability.
Applies to TREK™ RX 4.50mm and5.00mm sizes only, in addition to above:
With 4.5 mm and 5.0 mm balloon dilatation catheters, some increased resistance may be noted upon insertion or withdrawal into or out of the guiding catheter. Choosing a larger guiding catheter size may minimize this.
Applies to TREK™ OTW and MINI TREK™ II OTW (APPLIES TO ALL SIZES), in addition to above:
Bench testing was conducted with 0.014” (.36mm) constant diameter guide wires to establish guide wire compatibility. If another type of guide wire is selected with a different dimensional profile, the compatibility (e.g., wire resistance) should be considered prior to use.
Adverse Events (applies to all sizes)
Possible adverse effects include, but are not limited to, the following:
- Acute myocardial infarction
- Arrhythmias, including ventricular fibrillation
- Arteriovenous fistula
- Coronary artery spasm
- Coronary vessel dissection, perforation, rupture, or injury
- Death
- Drug reactions, allergic reaction to contrast medium
- Embolism
- Hemorrhage or hematoma
- Hypo / hypertension
- Infection
- Restenosis of the dilated vessel
- Total occlusion of the coronary artery or bypass graft
- Unstable angina
MAT-2109405 v2.0
StarClose SE™ Vascular Closure System

Indications for Use
The StarClose SE™ Vascular Closure System is indicated for the percutaneous closure of common femoral artery access sites while reducing times to hemostasis, ambulation, and dischargeability in patients who have undergone diagnostic endovascular catheterization procedures utilizing a 5F or 6F procedural sheath.
The StarClose SE™ Vascular Closure System is indicated for use to allow patients who have undergone diagnostic endovascular catheterization procedures to ambulate and be eligible for discharge as soon as possible after device placement.
The StarClose SE™ Vascular Closure System is indicated for the percutaneous closure of common femoral artery access sites while reducing times to hemostasis and ambulation in patients who have undergone interventional endovascular catheterization procedures utilizing a 5F or 6F procedural sheath.
Caution
Federal law restricts this device to sale by or on the order of a physician (or allied healthcare professionals, authorized by, or under the direction of, such physicians) who is trained in diagnostic and therapeutic catheterization procedures and who has been trained by an authorized representative of Abbott Vascular.
Prior to use, the operators must review the Instructions for Use and be familiar with the deployment techniques associated with the use of this device.
Contraindications
The StarClose SE™ Vascular Closure System is contraindicated for use in patients with known hypersensitivity to nickel-titanium.
Warnings
Do not use the StarClose SE™ Vascular Closure System if the packaging or sterile barrier has been previously opened or damaged or if the components appear to be damaged or defective.
DO NOT RESTERILIZE OR REUSE. The StarClose SE™ Vascular Closure System and accessories are intended for single use only.
Do not use the StarClose SE™ Vascular Closure System if the sterile field has been broken where bacterial contamination of the sheath or surrounding tissues may have occurred, since such a broken sterile field may result in infection.
Do not use the StarClose SE™ Vascular Closure System if the puncture site is located above the most inferior border of the inferior epigastric artery (IEA) and / or above the inguinal ligament based upon bony landmarks, since such a puncture site may result in a retroperitoneal hematoma. Perform a femoral angiogram to verify the location of the puncture site.
Do not use the StarClose SE™ Vascular Closure System if the puncture is through the posterior wall or if there are multiple punctures, since such punctures may result in a retroperitoneal hematoma.
Do not use the StarClose SE™ Vascular Closure System if the puncture site is located in the superficial femoral artery or the profunda femoris artery, since such puncture sites may result in a pseudoaneurysm, intimal dissection, or an acute vessel closure (thrombosis of small artery lumen). Perform a femoral angiogram to verify the location of the puncture site.
Precautions
- The StarClose SE™ Vascular Closure System should be used only by operators trained in diagnostic and interventional catheterization procedures who have been certified by an authorized representative of Abbott Vascular Inc.
- The StarClose SE™ Vascular Closure System is provided sterile and non-pyrogenic in unopened undamaged packaging. Products are sterilized with ethylene oxide and intended for single use only. Do not resterilize. Store in a cool, dry place.
- Prior to use, inspect the StarClose SE™ Vascular Closure System to ensure that the sterile packaging has not been damaged during shipment. Examine all components prior to use to verify proper function. Exercise care during device handling to reduce the possibility of accidental device breakage.
- As with all catheter-based procedures, infection is a possibility. Observe sterile technique at all times when using the StarClose SE™ Vascular Closure System. Employ appropriate groin management, as per hospital protocol, post-procedure and post-hospital discharge to prevent infection.
- Use a single wall puncture technique. Do not puncture the posterior wall of the artery.
- Do not use the StarClose SE™ Vascular Closure System to close vessels with diameters less than 5 mm.
- Do not deploy the Clip in areas of calcified plaque.
- The StarClose SE™ Vascular Closure System can be used ONLY with the StarClose Exchange System (included in the StarClose SE™ Vascular Closure System packaging).
- Do not advance or withdraw the StarClose SE™ Vascular Closure Device against resistance until the cause of that resistance has been determined. Excessive force used to advance or torque the StarClose SE™ device should be avoided, as this may lead to significant vessel damage and/or breakage of the device, which may necessitate interventional and/or surgical removal of the device and vessel repair.
MRI Safety Information
The StarClose Clip has been shown to be MR Conditional immediately following implantation. A patient with this implant can be scanned safely immediately after clip placement under the following conditions:
- Static magnetic field of 3 Tesla or less
- Spatial gradient magnetic field of 720 Gauss/cm or less
- Maximum MR system reported whole-body-averaged specific absorption rate (SAR) of 3 W/kg for 15 minutes of scanning.
In non-clinical testing, the StarClose Clip produced a temperature rise of 0.5°C at maximum MR system-reported whole-body-averaged specific absorption rate (SAR) of 3 W/kg for 15 minutes of MR scanning in a 3 Tesla MR system using a transmit/receive body coil.
The MR image quality may be compromised if the area of interest is in the exact same area or relatively close to the position of the StarClose Clip. Therefore, optimization of MR imaging parameters to compensate for the presence of this implant may be necessary.
Adverse Events
Potential adverse events that could be associated with the use of this device include:
- Major Vascular Complications (Composite)
- Vascular Injury Requiring Repair
- Surgery
- Angioplasty
- Ultrasound Guided Compression
- Thrombin Injection or Other Percutaneous Procedure
- New Ipsilateral Lower Extremity Ischemia
- Access Site-related Bleeding Requiring Transfusion
- Access Site-related Infection Requiring Intravenous Antibiotics or Prolonged Hospitalization
- Access Site-related Nerve Injury Requiring Intervention
- Death
- Minor Vascular Complications (Composite)
- Pseudoaneurysm
- Arteriovenous Fistula
- Hematoma (≥ 6 cm)
- Late Access Site-related Bleeding
- Transient Lower Extremity Ischemia
- Ipsilateral Deep Vein Thrombosis
- Transient Access Site-related Nerve Injury
- Access Site-related Vessel Injury
- Access Site Wound-related Dehiscence
- Access Site-related Bleeding Requiring ≥ 30 minutes to Re-achieve Hemostasis
- Localized Access Site Infection Treated with IM or Oral Antibiotics
- UADE
MAT-2114590 v3.0
Diamondback 360™ and Diamondback 360 Precision™ Coronary Orbital Atherectomy System

Including the Orbital Atherectomy Device (OAD) with GlideAssist™, Saline Pump, ViperWire Advance™ Coronary Guide Wire, and ViperWire Advance™ with Flex Tip Coronary Guide Wire
INDICATIONS
The Diamondback 360™ Coronary Orbital Atherectomy System (OAS) is a percutaneous orbital atherectomy system indicated to facilitate stent delivery in patients with coronary artery disease (CAD) who are acceptable candidates for PTCA or stenting due to de novo, severely calcified coronary artery lesions.
CONTRAINDICATIONS
Use of the OAS is contraindicated for use in the following situations:
- The ViperWire™ guide wire cannot pass across the coronary lesion.
- The target lesion is within a bypass graft or stent.
- The patient is not an appropriate candidate for bypass surgery, angioplasty, or atherectomy therapy.
- The patient has angiographic evidence of thrombus.
- The patient has only one open vessel.
- The patient has angiographic evidence of significant dissection at the treatment site.
- Women who are pregnant or children.
WARNINGS
- Do not use the OAS if the physician does not have experience in coronary angioplasty at their institution.
- Do not use the OAS if the physician does not have training on using the OAS. Contact a CSI representative for information on training.
- Do not use other commercially-available guide wires with the OAD. Only use the Model GWC-12325LG-FLP ViperWire Advance™ Coronary Guide Wire or GWC- 12325LG-FT ViperWire Advance™ Coronary Guide Wire with Flex Tip with the coronary OAD. The ViperWire™ guide wire is designed for use with all coronary OAD crown and shaft configurations.
- Never operate the OAD without normal saline and ViperSlide™ Lubricant. Continually flowing saline and ViperSlide Lubricant is required for cooling and lubricating the OAD during use in order to avoid overheating and permanent damage to the device and possible injury to the patient.
- Do not use the OAD or the ViperWire™ guide wire if their sterile package barriers are compromised or damaged.
- Do not use device during spasm of the vessel.
- Do not re-sterilize or re-use the OAD. If the OAD is re-sterilized or re-used, the OAD may not function properly potentially leading to serious infection and patient harm and/or death.
- Do not re-sterilize or re-use the ViperWire guide wire or the guide wire torquer. If the ViperWire™ guide wire or torquer is re-sterilized or re-used, the guide wire may not function properly potentially leading to serious infection and patient harm and/or death.
- Never use force to advance the spinning crown as vessel perforation may occur. If any resistance to crown travel is felt, reposition the crown away from the lesion, immediately stop treatment, and use fluoroscopy to assess the vessel for any complications. If it is confirmed there are no complications, reposition the device and advance and retract at a targeted rate of 1 to 3 mm per second.
- Use fluoroscopy to monitor and maintain spacing between the driveshaft and guide wire spring tip throughout the procedure. Always keep more than 5mm of spacing between the distal end of the OAD driveshaft and the proximal end of the guide wire spring tip. If the distance between the driveshaft tip and the ViperWire™ guide wire spring tip is insufficient, the driveshaft tip may contact the guide wire spring tip and result in dislodging the guide wire spring tip.
- Immediately stop using any OAS component should mechanical failure of any component occur before or during the atherectomy procedure. Using damaged components may result in OAS malfunction or patient injury.
- Immediately stop use of the OAD if the device stalls. Review for complications if a stall condition occurs. Do not change to high speed if device stalls on low speed.
- Note: If a stall occurs, the On/Off button is inactive for five seconds. If the On/Off button is pressed during this five second lockout period, the lockout period will begin again.
- Initial treatment for each lesion must start at low speed.
- Do not continue treatment if the wire or the device becomes subintimal.
- Do not operate the OAD if there is a bend, kink, or tight loop in the ViperWire™ guide wire. A bend, kink, or tight loop in the ViperWire™ guide wire may cause damage to and malfunctioning of the device during use.
- Performing treatment in excessively tortuous or angulated vessels or bifurcations may result in vessel damage or device failure requiring retrieval.
- Always keep the crown advancing or retracting, while it is orbiting, by continually moving the crown advancer knob to ensure corresponding (1:1) movement between the crown advancer knob and the orbiting crown.
- Do not start or stop orbiting of the crown when tight in a lesion.
- Once the OAD has reached full speed (as indicated by a stable pitch) continue to maintain a targeted travel rate of 1 to 3 mm per second, and do not exceed 10 mm per second. If the orbiting crown remains in one location it may lead to vessel damage.
- Maximum total treatment time should not exceed 5 minutes. If maximum total treatment time exceeds 5 minutes, the OAD shaft, crown, and ViperWire™ guide wire may begin to exhibit signs of wear and result in a device malfunction and possible injury to patient. A team member should track run time during use to verify total run time is not exceeded.
- Do not advance or retract the orbiting crown by advancing the OAD sheath or handle. Buckling of the ViperWire™ guide wire may occur resulting in vessel perforation or vascular trauma. Always advance the orbiting crown by using the crown advancer knob.
- Do not inject contrast solution into the OAD injection port. Device failure or patient harm may occur.
- Do not attempt aspiration through the OAD or saline line while placed within the body. If saline is pulled out through the OAD or saline line, air may enter the system.
- If air is noticed in the system while the OAD is within the body, discontinue treatment by pressing the OAS Pump power button and carefully remove the OAD driveshaft and crown from the introducer sheath/guide catheter.
- Do not allow body parts or clothing to come into contact with spinning components as the OAD orbits at very high speeds. Physical injury to the user or entanglement of clothing with the crown may occur.
- The OAS was only evaluated in severely calcified lesions; therefore the scientific evidence to support use of the OAS to treat other types of lesions/patients is limited.
- Do not spin the crown in GlideAssist™, with the guide wire brake lever in the unlocked position, without first securing the guide wire by holding it with fingers or by using the guide wire torquer. If using the guide wire torquer, ensure that it is securely fastened to the guide wire before starting to spin the crown. Failure to secure the guide wire when the brake is unlocked could allow the guide wire to spin while in GlideAssist™ mode which may result in patient harm.
PRECAUTIONS
- Do not use the OAD if there is damage to the OAD package or if the OAD has reached its shelf-life expiration date.
- If using an adjustable hemostasis valve with the guide catheter, close the hemostasis valve to minimize blood loss from around the guide catheter while still allowing the OAD sheath to slide through the hemostasis valve. Avoid excessive tightening of the hemostasis valve to prevent damaging the OAD catheter sheath. When inserting or removing the OAD crown or drive shaft through the hemostasis valve, use care not to deform the drive shaft.
- If crown and crown advancer knob movements are not moving correspondingly with one another (1:1 movement), retract and re-advance the crown into the lesion using a travel rate between 1 to 3 mm per second. Repeat retracting and advancing the crown into the lesion until crown to crown advancer knob movement correspondence is observed. If the knob and the crown are not moving together, the crown may be driven into the lesion with too much force and may result in the crown springing forward on exiting the lesion.
- Follow standard institution atherectomy policies and procedures, including those related to anticoagulation, channel blockers, and vasodilator therapy.
- Ensure fluoroscopy provides adequate visualization of the OAS system. Always use fluoroscopy to monitor the guide wire spring tip and driveshaft positions at all times throughout the procedure. If wire movement occurs, it is suggested to reposition the guide wire before advancing the device or continuing treatment.
- Applies to Diamondback 360™ Precision Coronary OAS only: Verify that contrast media injections are not above 400 psi and are not occurring during spinning of the crown.
- Applies to Diamondback 360™ Precision Coronary OAS only: If using a guide catheter smaller than 0.071 inches (1.80 mm), contrast media flow may be reduced.
- A temporary pacing lead may be necessary when treating lesions in the right coronary and circumflex arteries due to the possible occurrence of electrophysiological alternations.
- The risk of the occurrence of a dissection or perforation is increased in severely calcified lesions undergoing percutaneous treatment; therefore, on-site surgical back- up should be included as a clinical consideration. If onsite surgical back-up is not provided, then an agreement with an alternative hospital should be considered, in advance of the procedure, where the patient could be transferred in an emergency situation.
- Do not kink or crush the saline tubing as this will reduce the flow of saline and ViperSlide™ Lubricant to the OAD.
- Continually monitor and check the saline tubing and connections for leaks during the procedure.
- Do not spin the crown while advancing or retracting the crown within a guide catheter or tuohy. Damage to the guide catheter, tuohy, and/or OAD may occur.
- Ensure the OAD strain relief remains straight during atherectomy treatment. If the OAD strain relief does not remain straight, the shaft/sheath can kink.
- Do not sterilize the OAS pump. Sterilizing will damage the OAS pump. The OAS pump is intended to be used and maintained outside of the sterile field. Reference the Instructions for Use on cleaning and disinfecting the OAS pump.
- Do not allow fluid to leak onto electrical connections of the OAS pump.
- Do not spin the crown without a seated and supportive guide catheter
- When treating from a larger lumen to a smaller lumen, make sure the guide catheter is coaxial and that the tip of the OAD has entered the coronary artery to control the initial orbit before engaging the crown; engage the OAD tip into the tight stenosis until low speed has reached its treatment potential prior to initiating treatment with high speed.
- To relieve compression in the driveshaft, lock the crown advancer knob at 1cm from the full back position, advance device over wire to a position proximal from the lesion, deploy the guide wire brake, then unlock the crown advancer knob and move it fully proximal. If the OAD is started with existing compression in the driveshaft it may result in the crown springing forward.
- Do not flip contents of tray into sterile field as damage may occur. Components within tray must be carefully removed and placed into sterile field to avoid damage.
- Ejection fractions less than 25% have not been studied, use with low ejection fractions may require additional precautions due to compromised heart function.
POTENTIAL ADVERSE EVENTS
Potential adverse events that may occur and/or require intervention include, but are not limited to:
- Allergic reaction to medication/media/device components. Aneurysm. Angina (ischemic chest pain). Arrhythmias. Arteriovenous fistula. Bleeding. Bruising/hematoma. Cardiac/cardiopulmonary arrest. Cardiac/pericardial tamponade. Cerebrovascular accident (CVA). Death. Embolization, distal (air, tissue, thrombus, device). Emergent coronary artery bypass graft surgery (CABG). Failure to deliver the system to the intended locations. Fever. Heart failure/dysfunction. Hemorrhage, requiring transfusion. Hypotension/hypertension. Infection. Myocardial infarction. Pain. Pericardial effusion. Pseudoaneurysm. Restenosis of treated segment leading to revascularization. Renal insufficiency/failure. Shock (cardiogenic, hypovolemic). Slow flow or no reflow phenomenon. Stroke. Thrombus. Vessel closure, abrupt. Vessel injury, requiring surgical repair. Vessel dissection, perforation, rupture, or spasm. Vessel occlusion.
Diamondback 360™ and Diamondback 360 Precision™ Coronary Orbital Atherectomy System are manufactured and distributed by Cardiovascular Systems, Inc. (CSI). CSI is a subsidiary of the Abbott Group of Companies.
MAT-2303956 v1.0
Scoreflex‡ NC Scoring PTCA Catheter

INDICATIONS
The Scoreflex‡ NC Scoring PTCA Catheter is indicated for: Balloon dilatation of a de novo stenotic portion of a coronary artery and in-stent restenosis in coronary arteries in patients evidencing coronary ischemia for the purpose of improving myocardial perfusion.
CONTRAINDICATIONS
The use of the Scoreflex‡ NC Scoring PTCA Catheter is contraindicated in the following patient types:
- Patients with an unprotected left main coronary artery.
- Patients with coronary artery spasm in the absence of a significant stenosis.
WARNINGS
When using this type of device, the following warnings should be observed:
- This device is intended for single use only. Do not resterilize and/or reuse, as this can potentially result in compromised device performance and increased risk of cross-contamination.
- This balloon is not intended for the expansion or delivery of a stent.
- PTCA in patients who are not acceptable candidates for coronary artery bypass graft surgery require careful consideration, including possible hemodynamic support during PTCA, as treatment of this patient population carries special risk.
- To reduce the potential for vessel damage, the inflated diameter of the balloon should approximate the diameter of the vessel just proximal and distal to the stenosis.
- When the catheter is exposed to the vascular system, it should be manipulated while under high-quality fluoroscopic observation. Do not advance or retract the catheter unless the balloon is fully deflated under vacuum. If resistance is met during manipulation, determine the cause of the resistance before proceeding. Applying excessive force to the catheter can result in tip or catheter breakage, catheter kink, or balloon separation.
- Do not twist the catheter shaft in excess of 180 degrees when the tip is constrained.
- Balloon pressure should not exceed the rated burst pressure (RBP) indicated on the package. The rated burst pressure is based on the results of in vitro testing. At least 99.9 percent of the balloons, (with a 95 percent confidence) will not burst at or below their rated burst pressure. Use of a pressure monitoring device is recommended to prevent over pressurization.
- To reduce the potential for air embolus into the vessel, use only the recommended balloon inflation medium. Never use air or any gaseous medium to inflate the balloon.
- Do not re-straighten a kinked hypotube; straightening a kinked metal shaft may result in breakage of the shaft.
- PTCA should only be performed at hospitals where emergency coronary artery bypass graft surgery can be quickly performed in the event of a potentially injurious or life-threatening complication.
PRECAUTIONS
- Use the catheter prior to the “Use By” date specified on the package.
- Prior to angioplasty, the catheter should be examined to verify functionality and ensure that its size and shape are suitable for the specific procedure for which it is to be used.
- The catheter system should be used only by physicians trained in percutaneous transluminal coronary angioplasty.
- During the procedure, appropriate anticoagulant and coronary vasodilator therapy must be provided to the patient as needed. After the procedure, anticoagulant therapy should be continued for a period of time as determined by the physician.
- Never advance the Scoreflex‡ NC Scoring PTCA Catheter without the guidewire extending from the tip.
- Do not use oil-based contrast medium, organic solvents, or alcohols; there is a possibility of catheter leak, damage, or lubrication loss.
- The balloon deflation time has been established as 15 seconds based on in vitro bench testing results.
- Do not reinsert the PTCA catheter into the coil dispenser after procedural use.
- Discard all disposable devices used during this procedure per local requirements for medical device waste disposal.
ADVERSE EVENTS
Adverse events that may be associated with the use of this product include, but are not limited to, the following:
- Death
- Acute myocardial infarction
- Total occlusion of the coronary artery
- Coronary vessel dissection, perforation, rupture, or injury
- Acute vessel closure
- Restenosis of the dilated vessel
- Unstable angina
- Stroke, air embolism and embolization of fragmentation of thrombotic or atherosclerotic material
- Arrhythmias, including ventricular fibrillation
- Hypertension
- Hypotension
- Coronary artery spasm
- Hemorrhage or hematoma
- Arteriovenous fistula
- Drug reactions, allergic reaction to contrast medium
- Infection
- Need for blood transfusion
CAUTION: This product is intended for use by or under the direction of a physician. Prior to use, reference the Instructions for Use, inside the product carton (when available), at manuals.eifu.abbott or at eifu.orbusneich.com for more detailed information on Indications, Contraindications, Warnings, Precautions and Adverse Events. This material is intended for use with healthcare professionals only.
Scoreflex‡ NC Scoring PTCA Catheter is manufactured by OrbusNeich Medical Group Holdings Limited or its affiliates and distributed by Cardiovascular Systems, Inc. (CSI). CSI is a subsidiary of the Abbott Group of Companies.
MAT-2303959 v2.0
Sapphire‡ NC24 Coronary
Dilatation Catheter

INDICATIONS
The Sapphire‡ NC24 Coronary Dilatation Catheter is indicated for:
- Balloon dilatation of the stenotic portion of a coronary artery or bypass graft stenosis in patients evidencing coronary ischemia for the purpose of improving myocardial perfusion.
- Balloon dilatation of a coronary artery occlusion for the treatment of acute myocardial infarction.
- In-stent restenosis.
- Post-delivery expansion of balloon expandable coronary stents.
CONTRAINDICATIONS
The use of Sapphire‡ NC24 Coronary Dilatation Catheter is contraindicated in the following patient types:
- Patients with an unprotected left main coronary artery.
- Patients with coronary artery spasm in the absence of a significant stenosis.
WARNINGS
When using this type of device, the following warnings should be observed:
- To reduce the potential for vessel damage, the inflated diameter of the balloon should approximate the diameter of the vessel just proximal and distal to the stenosis.
- PTCA in patients who are not acceptable candidates for coronary artery bypass graft surgery require careful consideration, including possible hemodynamic support during PTCA, as treatment of this patient population carries special risk.
- When the catheter is exposed to the vascular system, it should be manipulated while under high quality fluoroscopic observation. Do not advance or retract the catheter unless the balloon is fully deflated under vacuum. If resistance is met during manipulation, determine the cause of the resistance before proceeding.
- Balloon pressure should not exceed the Rated Burst Pressure (RBP) indicated on the package. The RBP is based on the results of in vitro testing. At least 99.9 percent of the balloons, (with a 95 percent confidence) will not burst at or below their rated burst pressure. Use of a pressure monitoring device is recommended to prevent over pressurization.
- PTCA should only be performed at hospitals where emergency coronary artery bypass graft surgery can be quickly performed in the event of a potentially injurious or life-threatening complication.
- Use only the recommended balloon inflation medium. Never use air or any gaseous medium to inflate the balloon.
- This device is designed and intended for single use only. DO NOT reprocess, re-sterilize and/or reuse. Reuse of single-use devices creates a potential risk of patient or user infections. Reuse may lead to impairment of functional performance. Infections and/or limited performance of the device may lead to injury, illness or death in the patient.
- Do not re-straighten a kinked hypotube; straightening a kinked metal shaft may result in breakage of the shaft.
PRECAUTIONS
- Use the catheter prior to the "Use By" date specified on the package.
- Prior to angioplasty, the dilatation catheter should be examined to verify functionality and ensure that its size is suitable for the specific procedure for which it is being used.
- The catheter system should be used only by physicians trained in percutaneous transluminal coronary angioplasty.
- During the procedure, appropriate anticoagulant and coronary vasodilator therapy must be provided to the patient as needed. After the procedure, anticoagulant therapy should be continued for a period of time as determined by the physician.
- Do not re-insert the PTCA catheter into the coil dispenser after procedural use.
- The design and construction of these catheters do not provide the user with distal pressure monitoring capability.
- Discard all disposable devices used during this procedure per local requirements for medical device waste disposal.
- Do not use oil-based contrast medium, organic solvents or alcohols; there is a possibility of catheter leak, damage or lubrication loss.
- Use with caution for procedures involving calcified lesions due to the abrasive nature of these lesions.
POTENTIAL COMPLICATIONS AND ADVERSE EVENTS
Potential complications and adverse effects due to the use of this product include, but are not limited to, the following:
- Death
- Acute myocardial infarction
- Acute Vessel Closure
- Total occlusion of the coronary artery or bypass graft
- Coronary vessel dissection, perforation, rupture, or injury
- Restenosis of the dilated vessel
- Hemorrhage or hematoma
- Unstable angina
- Arrhythmias, including ventricular fibrillation
- Drug reactions, allergic reaction to contrast medium
- Hypo/hypertension
- Infection
- Coronary artery spasm
- Arteriovenous fistula
- Stroke, air embolism and embolization of fragmentation of thrombotic or atherosclerotic material
CAUTION: This product is intended for use by or under the direction of a physician. Prior to use, reference the Instructions for Use, inside the product carton (when available), at manuals.eifu.abbott or at eifu.orbusneich.com for more detailed information on Indications, Contraindications, Warnings, Precautions and Adverse Events. This material is intended for use with healthcare professionals only.
MAT-2400959 v2.0
Sapphire‡ II Pro Balloon
Dilatation Catheter

INDICATIONS
The Sapphire‡ II PRO Dilatation Catheter (Ø1.0-1.25mm configurations) is indicated for:
- balloon pre-dilatation of a stenotic portion of a coronary artery or bypass graft stenosis (≥70% stenosis) for the purpose of improving myocardial perfusion.
The Sapphire‡ II PRO Dilatation Catheter (Ø1.5-4.0mm configurations) is indicated for:
- balloon dilatation of the stenotic portion of a coronary artery or bypass graft stenosis in patients evidencing coronary ischemia for the purpose of improving myocardial perfusion;
- balloon dilatation of a coronary artery occlusion for the treatment of acute myocardial infarction.
The Sapphire‡ II PRO Dilatation Catheter is also indicated for:
- percutaneous transluminal angioplasty in the peripheral vasculature, including renal, femoral, popliteal, infra-popliteal, tibial, and peroneal arteries.
CONTRAINDICATIONS
The use of the Sapphire‡ II PRO Dilatation Catheter is contraindicated:
- for use in patients with an unprotected left main coronary artery.
- for use in patients with coronary artery spasm in the absence of a significant stenosis.
- for use in the neuro vasculature.
- where there is the inability to cross the target lesion with a guidewire.
WARNINGS
When using this type of device, the following warnings should be observed:
- This device is intended for single use only. Do not resterilize and/or reuse, as this can potentially result in compromised device performance and increased risk of cross-contamination.
- The safety and effectiveness of this balloon catheter for the treatment of in stent restenosis (ISR) has not been established.
- This balloon is not intended for the expansion or delivery of a stent.
- To reduce the potential for vessel damage, the inflated diameter of the balloon should approximate the diameter of the vessel just proximal and distal to the stenosis.
- PTCA in patients who are not acceptable candidates for coronary artery bypass graft surgery require careful consideration, including possible hemodynamic support during PTCA, as treatment of this patient population carries special risk.
- When the catheter is exposed to the vascular system, it should be manipulated while under high-quality fluoroscopic observation. Do not advance or retract the catheter unless the balloon is fully deflated under vacuum. If resistance is met during manipulation, determine the cause of the resistance before proceeding. Applying excessive force to the catheter can result in separation of the tip or balloon.
- Balloon pressure should not exceed the rated burst pressure (RBP) indicated on the package. The rated burst pressure is based on the results of in vitro testing. At least 99.9 percent of the balloons, (with a 95 percent confidence) will not burst at or below their rated burst pressure. Use of a pressure monitoring device is recommended to prevent over pressurization.
- To reduce the potential for air embolus into the vessel, use only the recommended balloon inflation medium. Never use air or any gaseous medium to inflate the balloon.
- For the rapid exchange catheter, do no re-straighten a kinked hypotube; straightening a kinked metal shaft may result in breakage of the shaft.
- PTCA should only be performed at hospitals where emergency coronary artery graft surgery can be quickly performed in the event of a potentially injurious or life-threatening complication.
PRECAUTIONS
- Use the catheter prior to the “Use By” date specified on the package.
- Prior to angioplasty, the catheter should be examined to verify functionality and ensure that its size and shape are suitable for the specific procedure for which it is to be used.
- The catheter system should be used only by physicians trained in percutaneous transluminal coronary or peripheral angioplasty.
- During the procedure, appropriate anticoagulant and vasodilator therapy must be provided to the patient as needed. After the procedure, anticoagulant therapy should be continued for a period of time as determined by the physician.
- Do not reinsert the catheter into the coil dispenser after procedural use.
- Discard all disposable devices used during this procedure per local requirements for medical device waste disposal.
- Do not use oil-based contrast medium, organic solvents or alcohols; there is a possibility of catheter leak, damage, or lubrication loss.
- The balloon deflation time has been established as 15 seconds based on in vitro bench testing results.
- Use with caution for procedures involving calcified lesions due to the abrasive nature of these lesions.
ADVERSE EVENTS
Adverse effects due to the use of this product include, but are not limited to, the following:
- Acute myocardial infarction
- Acute or subacute thrombosis
- Acute vessel closure
- Allergic reaction to device, contrast medium, or medication
- Aneurysm
- Arrhythmias, including ventricular fibrillation
- Arteriovenous fistula
- Coronary artery spasm
- Death
- Dissection (perforation, rupture, or injury) of the vessel
- Hemorrhage or hematoma
- Hypertension
- Hypotension
- Infection
- Restenosis of the dilated vessel
- Stroke, air embolism and embolization of fragmentation of thrombotic or atherosclerotic material
- Total occlusion of the artery or bypass graft
- Unstable angina
CAUTION: This product is intended for use by or under the direction of a physician. Prior to use, reference the Instructions for Use, inside the product carton (when available), at manuals.eifu.abbott or at eifu.orbusneich.com for more detailed information on Indications, Contraindications, Warnings, Precautions and Adverse Events. This material is intended for use with healthcare professionals only.
MAT-2400936 v2.0