Better Treatment Starts With An Accurate Diagnosis
To discover the root cause of persistent angina, patients may need an accurate diagnosis for Coronary Microvascular Dysfunction (CMD) that requires more than the angiogram alone.1 Comprehensive physiology testing of both the epicardial arteries and microcirculation can help provide a clear diagnosis to guide treatment and improve patient outcomes.2
The Microvasculature Can Have a Major Clinical and Economic Impact
The microcirculation carries far more myocardial blood volume compared to the epicardial arteries. CMD can be defined as impaired blood flow to the microcirculation, which is largely responsible for the regulation and distribution of blood flow to the myocardium.1
Ischemia With No Obstructed Coronary Arteries (INOCA) is Not Benign: The Effect On Clinical Outcomes
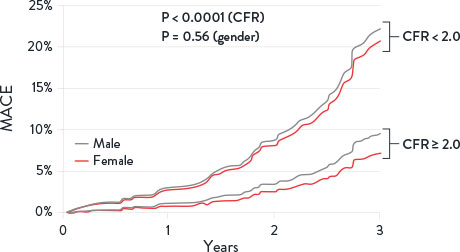
Patients with INOCA can be diagnosed for CMD by measuring Index of Microcirculatory Resistance (IMR) and Coronary Flow Reserve (CFR).3 Patients with abnormal CFR have an increase in major adverse cardiac events (MACE) including:
- Myocardial infarction1
- Stroke1
- Heart failure1,3
- Cardiovascular death1
Additionally, these patients have an increase in diastolic dysfunction and cardiac death.4
Coronary Flow Reserve Associated with MACE Risks1
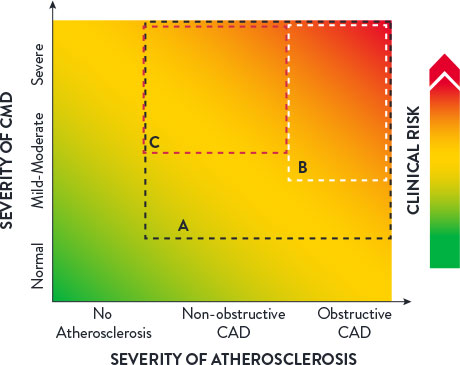
The clinical spectrum of CMD may be characterized by three factors:1
- The severity of CMD
- The degree of atherosclerosis
- Any associated clinical risks
Clinical Spectrum of CMD1
The Impact On Healthcare Costs
A clear, accurate CMD diagnosis can help reduce healthcare resource consumption.5
- For U.S. patients with INOCA symptoms, the economic cost of ineffective treatment is $13,977 per patient annually due to absenteeism (inability to go to work) and presenteeism (productivity loss at work).6
- An economic analysis of the CorMicA study showed that a comprehensive physiology assessment is cost-effective compared to standard care (medical therapy and cardiac rehabilitation care) at 1-year follow-up.7
- In fact, an accurate CMD diagnosis can help reduce healthcare resource consumption,8 resulting in lower costs for hospitals and patients9 with a savings from $2,100 (Netherlands) to $7,300 (U.S.) per hospitalization avoided (2017 costs).10
INOCA Patient Identification
40-60% of all elective patients undergoing angiography suffer from INOCA. Up to half of this patient population might have angina due to CMD.11,12
- Angina post-PCI occurs in 20-30% of patients at 1-year and may be caused by CMD.13
- CMD predominantly affects women, having been detected in up to 50% of women presenting with chest pain. A definitive diagnosis is critical as women with this condition are at an increased risk of cardiovascular events in the future.14,15
Symptoms of CMD can include:16
- Discomfort in the left arm, jaw, neck, back or abdomen associated with chest pain
- Shortness of breath
- Tiredness and lack of energy
ASSESSING PATIENTS
Guide to Identifying CMD Patients
Understanding the symptoms may help you determine if your patient could benefit from comprehensive physiology testing. Patients suffering from CMD may include:8
- Patients suffering from angina whose coronary arteries appear clear under angiography
- Patients suffering from angina post-PCI
- Patients with a negative stress test but suffering from angina
- Patients presenting to the ER with chronic angina
- Female patients suffering from angina
Other symptoms may include chest pain, shortness of breath, and more.
Helping Patients
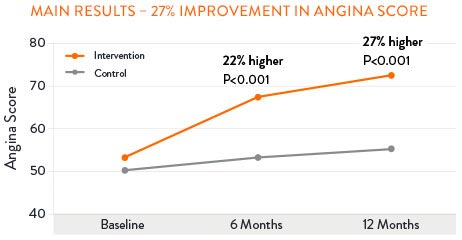
The CorMicA (Coronary Microvascular Angina) study revealed that patients may benefit when CMD is accurately diagnosed and appropriately treated. 27% of patients saw improvement in angina severity at 1 year with optimized medical therapy.17
Sustained Angina Improvement with CMD Treatment17,†
PressureWire™ X Guidewire with the CoroFlow‡ Cardiovascular System is the only* solution for the catherization laboratory able to assess both the epicardial arteries and the microvasculature that can give patients the accurate diagnosis that they deserve.17,18,19
Connect with your partnering referring physician to discuss how your access to the PressureWire™ X Guidewire and CoroFlow‡ Cardiovascular System can benefit their patients with angina and no angiographic abnormalities.
Learn more about PressureWire™ X Guidewire and CoroFlow‡ Cardiovascular System.

*With Index of Microcirculatory Resistance (IMR), Coronary Flow Reserve (CFR), Fractional Flow Reserve (FFR) and Resting Full-Cycle Ratio (RFR).
†According to the Seattle Angina Questionaire score.
References
- Taqueti, VR. et al. Coronary microvascular disease pathogenic mechanisms and therapeutic options: JACC state-of-the-art review. J Am Coll Cardiol. 2018;72:2625–2641.
- Lee, B. et al. Invasive evaluation of patients with angina in the absence of obstructive coronary artery disease. Circulation. 2015;131;10540-1060
- Gulati, MI., et al. 2021 AHA/ALL Guideline for the Evaluation and Diagnosis of Chest Pain. Circulation 2021;1440368-454.
- Knuuti, J., et al. 2019 ESC Guidelines for the diagnosis and management of chronic coronary syndromes. European Heart Journal 2020:41,407-477.
- Lee, B., et al. Invasive evaluation of patients with angina in the absence of obstructive coronary artery disease. Circulation. 2015:131:1054-1060.
- Schumann, CL., et al. Functional and economic impact of INOCA and influence of coronary microvascular dysfunction. JACC Cardiovascular Imaging 2021; 14: 1369-79.
- Heggie, R., et al. A cost-effectiveness analysis of the BHF CorMicA Trial. Interventional Journal of Cardiology 2021.
- Kunadian, V., et al. EAPCI Expert Consensus. Eur Heart J 2020;0:1-21.
- Reriani, M., et al. Coronary endothelial function testing may improve long-term quality of life in subjects with microvascular coronary endothelial dysfunction. Open Heart. 2019 6:8000870.
- Omerovic, E., et al. FFR-Guided Complete Revascularization During Primary Angioplasty: Effects on Societal Costs. EuroPCR 2017.
- Patel, M., et al. (2010). Low diagnostic yield of elective coronary angiography. The New England Journal of Medicine. 2010; 363;498.
- Maas, A. et al. Microvascular angina: diagnosis, assessment, and treatment. EMJ Int Cardiol. 2019; 7[Suppl 1]2-17.
- Jeremias, et al. DEFINE PCI. TCI 2019.
- Kuruvilla, S., & Kramer, C. MI. (2013). Coronary microvascular dysfunction in women: an overview of diagnostic strategies. Expert review of cardiovascular therapy, 11(11), 1515-1525.
- Garcia, M., et al. (2016). Cardiovascular Disease in Women: Clinical Perspectives. Circulation Research, 118(8), 1273-1293.
- Mayo Clinic webpage: Small vessel disease accessed on June 2022 at https://www.mayoclinic.org/diseases-conditions/small-vessel-disease/symptoms-causes/syc-20352117.
- Ford, TJ. et al. 1-year outcomes of angina management guided by invasive coronary function testing (CorMicA). JACC Intv. 2020;13:33-45.
- PressureWire™ X Guidewire Instructions for Use (IFU). Coroflow‡ Cardiovascular System (IFU). Refer to IFUs for additional information.
- Pijls, NH, et al. Fractional Flow Reserve Versus Angiography for Guiding Percutaneous Coronary Intervention in Patients with Multivessel Coronary Artery Disease. 2-Year Follow-Up of the FAME (Fractional Flow Reserve Versus Angiography for Multivessel Evaluation) Study. JACC. 2010; 56(3): 177-184.
MAT-2311270 v1.0
Coroventis‡ CoroFlow‡ Cardiovascular System

Indications: CoroFlow‡ is indicated to provide hemodynamic information for use in the diagnosis of patients with cardiovascular diseases.
CoroFlow‡ is intended for use in catheterization and related cardiovascular specialty laboratories to compute and display various physiological parameters based on the output from one or more measuring devices.
Contraindications: The system has no patient alarm functions. Do not use for cardiac/vital signs monitoring.
Warnings:
- If CoroFlow‡ is used together with 3rd party infusion catheters for assessment of Absolute Flow and Resistance, ensure that the maximum infusion rate per manufacturers instruction is not exceeded or vessel injury may occur.
- Do not use the CoroFlow‡ Cardiovascular System if there is reason to believe the system's security has been compromised or if the system was unaccounted for a period of time (i.e. misappropriated, modified or tampered with).
- Do not leave the CoroFlow‡ Cardiovascular System unattended when logged in as a PC Administrator.
- To protect the privacy and security of sensitive information, including electronic protected health information (EPHI), and to protect the integrity of the system itself, the system should be located in a physically secure, access-controlled environment.
- To protect the privacy and security of sensitive information, including electronic protected health information (EPHI), the PC on to which CoroFlow‡ is installed must be configured according to the Installation Instructions in this manual. Failure to configure the PC correctly may result in increased risk for unauthorized release of protected health information. Windows settings include:
- Activation and configuration of restricted user Access
- Activation of Windows Firewall and blocking of network connections
- Activation of Windows Bitlocker drive encryption
- Activation of Windows Secure Boot
- Activation of Windows Anti-Virus scanning and ransomware protection. Ensure CoroFlow‡ is added in the list of trusted applications.
- Activation of Windows update
- Disable unused interfaces
- Use of this equipment adjacent to or stacked with other equipment should be avoided because it could result in improper operation. If such use is necessary, this equipment and the other equipment should be observed to verify that they are operating normally.
- Use of accessories, transducers and cables other than those specified or provided by Coroventis‡ could result in increased electromagnetic emissions or decreased electromagnetic immunity of this equipment and result in improper operation.
- Portable RF communications equipment (including peripherals such as antenna cables and external antennas) should be used no closer than 30 cm (12 inches) to any part of CoroFlow‡, including cables specified by Coroventis‡. Otherwise, degradation of the performance of this equipment could result.
Precautions:
- The PC and CoroHub‡ shall not be placed within the patient environment (1.5 m from patient).
- For operation of other devices used in conjunction with CoroFlow‡ consult the IFU for each of these devices for details on indication, handling and safety information.
- It is recommended to ensure local routines for data backup of stored recordings. CoroFlow‡ does not create backup of stored data.
- Always check minimum performance requirement on PC to ensure compatibility with CoroFlow‡.
- It is recommended to install CoroFlow‡ on a PC with backup battery to avoid interruption in case of power failure.
- Always manually review and confirm valid cursor positions and detected heart beats.
- Ensure that Pa and Pd pressure waveforms are aligned in phase and offset after equalization, or indices can be mis-calculated.
- Confirm that the correct Wi-Box is selected by manually matching the Wi-Box ID number with the Wi-Box in the lab.
- Changing parameter settings outside of default values may affect measurement performance, only for research purposes.
- Only to be used by healthcare professionals.
- Using a network location to store data may cause previously unidentified risks if the network malfunctions.
- No modification or tampering with CoroFlow‡ is permitted.
- CoroFlow‡, including accessories and components, shall not be used if it has been subject to damage.
- The assembly of medical electrical systems and modifications during the actual service life require evaluation to the requirements according to IEC 60601-1 standard series.
- CoroHub‡ does not have any serviceable parts and require no field maintenance. No modification or tampering with CoroHub‡ is permitted.
- CoroHub‡ shall not be immersed in liquid.
- CoroHub‡ shall not be used if it has been subject to damage.
- PPG values may be non-unique and different combinations or focal/diffuse disease may result in the same PPG value.
- Direct connection to a non-secure network, like the internet, may interfere with correct operation and/or result in inappropriate access to patient information. Furthermore, it should be noted that reconfiguring a used network may lead to inability to import patient as well as export examination data, ultimately leading to a risk of loss of patient and examination data. To avoid this problem Coroventis‡ recommends verifying network settings in the system setup after each change. The same caution is relevant regarding connection to DICOM.
- Always confirm valid pressure tracings, marker positions and selected beats.
- Resetting CoroHub‡ will reset PressureWire connections and Zeroing/Equalization parameters.
MAT-2007904 v4.0
PressureWire™ X Guidewire

Indications: The PressureWire™ X Guidewire is indicated to direct a catheter through a blood vessel and to measure physiological parameters in the heart and in the coronary and peripheral blood vessels. Physiological parameters include blood pressure. The PressureWire™ X Guidewire can also measure blood temperature.
Contraindications: This guidewire is contraindicated for use in the cerebral vasculature.
Warnings:
- No modification of this device is allowed.
- The PressureWire™ X Guidewire is supplied sterile. Discard the guidewire if the pouch is opened or damaged, compromising the sterile barrier. The guidewire is designed for single use only and shall not be reused or resterilized. Adverse effects of using a non-sterile or resterilized guidewire may include, but are not limited to:
- Local and/or systemic infection
- Mechanical damage
- Inaccurate readings
- Observe all guidewire movements. Whenever the guidewire is moved or torqued, the tip movement should be examined under fluoroscopy. Never push, withdraw, or torque the guidewire if it meets resistance or without observing corresponding movement of the tip, otherwise vessel/ventricle trauma may occur.
- Torquing or excessive manipulation of the guidewire in a sharp bend, against resistance, or repeated attempts to cross a total vessel occlusion may:
- Cause dissection or perforation of blood vessels
- Cause vessel spasm
- Damage and/or fracture the guidewire
- When introducing the guidewire, flush the catheter and administer anticoagulation as for a standard catheterization procedure or clotting may occur.
- Do not use the guidewire in the ventricles if the patient has a prosthetic mechanical or biological valve. It may result in damage to both the prosthesis and the guidewire, which may cause injury or death.
- Use of the PressureWire™ X Guidewire in conjunction with interventional devices with a short rapid exchange may result in a folded or fractured guidewire.
- High frequency surgical devices must not be used on a patient at the same time as the guidewire.
Precautions:
- The PressureWire™ X Guidewire is a delicate instrument and should be handled carefully.
- Make sure that the transmitter is kept dry to ensure accurate pressure and/or temperature readings. Inaccurate readings may necessitate device replacement.
- Do not use the guidewire in conjunction with atherectomy catheters. It may damage the guidewire.
- Do not withdraw or manipulate the guidewire in a sharp-edged object. It may result in abrasion of the guidewire coating.
- Factors that may affect the accuracy of the diagnostic information include, but are not limited to:
- Improper placement of the aortic pressure sensor.
- Failure to achieve maximum coronary and myocardial hyperemia in FFR procedures.
- Blood flow affected by the position of interventional devices, such as balloon catheters.
- Guidewire readings may be affected by defibrillation. Rezero the guidewire after defibrillation use.
- Do not measure pressure when the guidewire sensor element is in a sharp bend or in contact with atrial or ventricular walls. It might result in pressure artifacts.
- Do not use the PressureWire™ X Guidewire together with another guidewire, for so called jailed wire technique, due to difficulty in guidewire withdrawal and possible guidewire entrapment.
- Store at room temperature (15°C – 25°C) in a dry and dark place.
Potential Adverse Events: Potential complications which may be encountered during all catheterization procedures include, but are not limited to: vessel dissection or occlusion, perforation, embolus, spasm, local and/or systemic infection, pneumothorax, congestive heart failure, myocardial infarction, hypotension, chest pain, renal insufficiency, serious arrhythmias, or death.
In addition, this device has a coating containing Polyethylene Glycol (PEG); potential allergic reactions (anaphylaxis) may occur during the interventional procedure if the patient is allergic to PEG.
MAT-2103599 v2.0

