Experience the OCT difference.
Request your Abbott Sales rep today.
OCT removes ambiguities in calcified lesions enabling proper stent expansion to achieve optimal results
Calcium is associated with decreased procedural success and stent underexpansion, resulting in adverse clinical outcomes.1
Presence and severity of coronary artery calcification is growing; up to 25% of patients, or 1 in 4, have moderate to severe calcium.2 If left undiagnosed and untreated, coronary artery calcification adversely impacts PCI outcomes.3
- Calcified lesions limit stent expansion, which is a major predictor of stent failure, such as stent thrombosis and restenosis.1
- Achieving optimal expansion is proven to reduce rates of major adverse cardiac events during PCI.4
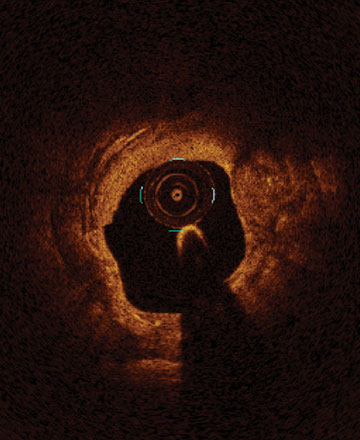
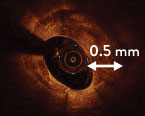
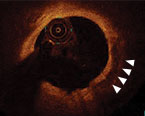
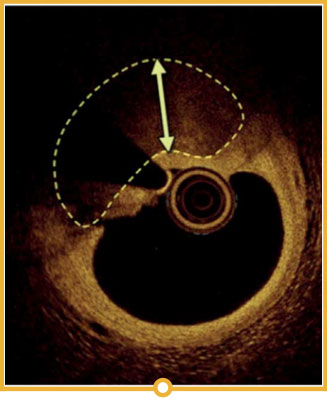
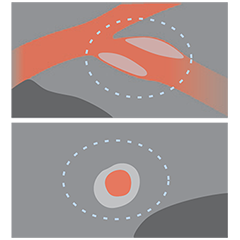
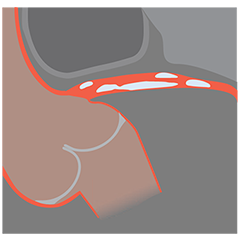
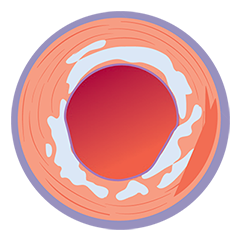
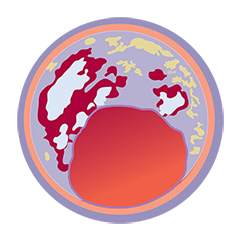
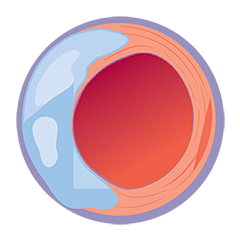
From left to right: Superficial almost 360 degree calcium; Calcific nodule from 12-3 o’clock and from 8-10 o’clock; Superficial 360 degree concentric calcium that’s fractured at 3, 6 and 9 o’clock.
OCT imaging enables effective visualization and quantification of coronary calcification characteristics which informs optimal lesion preparation strategy.1
OCT workflow, MLD MAX guides a user through treatment decisions for pre- and post- PCI. The first step of the workflow is to assess Morphology (M) to understand what type of plaque you are dealing with and how to best prepare the vessel before stenting. In calcified lesions, this assessment helps to determine the type of calcific plaque and its severity.

In LightLab Clinical Initiative,5 physicians changed lesion prep strategy in nearly 1/3 of lesions after they assessed lesion morphology and severity with OCT. When a change in vessel prep strategy occurred, calcification was the predominant morphology as seen with OCT.
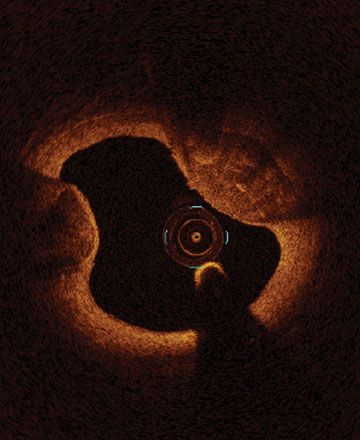
In the LightLab case, pre-PCI angio assessment and planned treatment approach (left image) was changed after performing pre-PCI OCT (right image).
The impactful changes include:
- Severity of lesion calcification angiographically underestimated.
- Vessel preparation strategy updated to Non-Compliant Balloon and Rotational Atherectomy instead of using the Compliant Balloon.
- Stent size changed by additional 6mm in size from the originally planned by angio assessment
Morphology:
Calcified Mid LAD lesion (Type B)
Hemodynamically significant
Length:
30 mm
Diameter:
3.0 mm Distal, 3.5 mm Proximal
Vessel Prep Planned: Compliant Balloon
Treatment planned: 3.0 mm x 32 mm stent
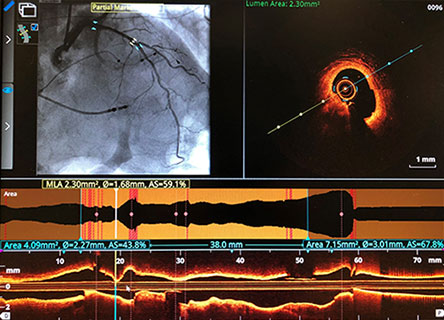
Morphology:
Calcified Mid LAD lesion (Type B)
Length:
38 mm
Diameter:
2.82 mm Distal EEL, 3.75 mm Proximal EEL
Minimum Lumen Area: 2.3 mm²
OCT Vessel Prep Planned: Non-Compliant Balloon, Rotational Atherectomy
Treatment planned: 3.0 mm x 38 mm stent
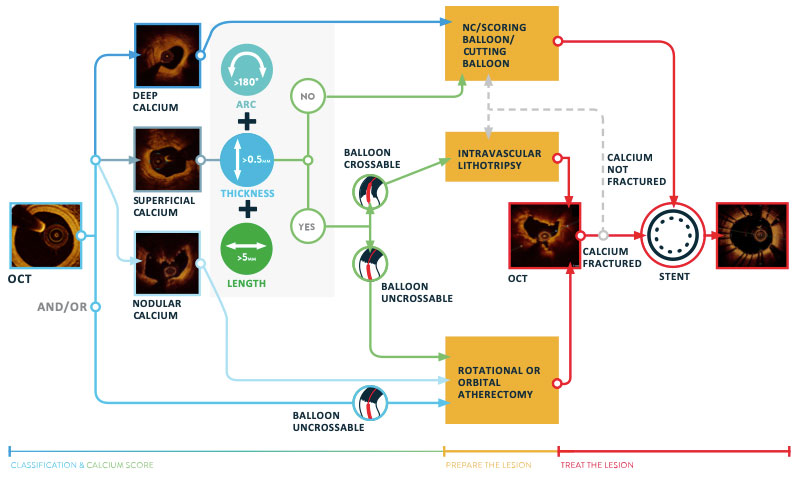
OCT classification of calcium
The use of intravascular imaging allows for more specific characterization and quantification of calcification compared to angiographic calcium classification as mild, moderate, or severe.
OCT helps to classify calcium into deep, superficial and nodular, as well as eccentric or concentric calcium. Morphology, and calcium, assessment is performed in the first step of the MLD MAX workflow. M- Morphology, is an important factor in determining the optimal treatment approach because different types of calcium require a different treatment technique.1

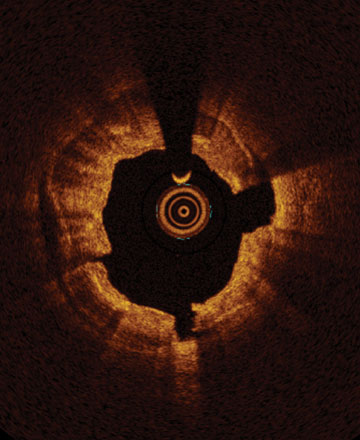
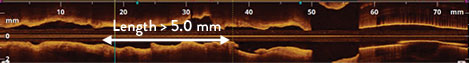
OCT calcium score: Rule of 5s
Measuring calcium depth with an OCT-based calcium scoring algorithm can help identify calcific lesions that would benefit from plaque modification before stent implantation.6 This algorithm looks at calcium thickness, calcium angle and calcium length which are among the most important parameters used to predict the need and success of calcium modification devices.
- Thickness >0.5 mm
- Angle >50% vessel arc
- Length >5 mm
Lesions at risk of stent under-expansion have a calcium score of 4:6
OCT-BASED CALCIUM VOLUME INDEX SCORE
≤ 90° 0 point
90° < Angle ≤ 180° 1 point
> 180° 2 points
≤ 0.5 mm 0 point
> 0.5 mm 1 point
≤ 5.0 mm 0 point
> 5.0 mm 1 point
TOTAL SCORE = 0-4 POINTS
Rule of 5s
1 0.5 mm thickness
2 50% vessel arc
3 5.0 mm long
Evaluation of calcium thickness is key in predicting stent expansion.7 With IVUS, the sound waves bounce off calcium and create a dark shadow. With OCT, the light can penetrate calcium thus evaluate its thickness.7


How to diagnose and treat calcified lesions with OCT
- Start PCI with the MLD MAX workflow
- Assess Morphology (M) to determine the type of plaque
- For calcific plaque, apply OCT-guided treatment of Calcified lesions algorithm.1 The algorithm guides physicians from assessment of calcific burden to lesion preparation and optimal stent expansion.
OCT guidance enables accurate identification of calcium characteristics and vessel morphologies aiding in proper lesion preparation strategies influencing successful PCI and decreased future revascularizations.
How does OCT imaging compare to other modalities used for calcified lesions?
OCT is the best imaging modality to detect, localize and quantify coronary calcium.8
Coronary angiography, coronary computed tomography (CT), intravascular ultrasound (IVUS), radiofrequency (RF), intravascular ultrasound-virtual histology (IVUS-VH), and optical coherence tomography (OCT) can all detect and attempt to localize and quantify calcium, albeit with very different diagnostic accuracies, as concluded by Gary Mintz after 20 years of intravascular imaging studies of the relationship between calcium and coronary atherosclerosis.8
| Coronary Angiography | CT | IVUS | RF-IVUS (IVUS-VH) | OCT | |
|---|---|---|---|---|---|
| IMAGING MODALITIES |  | 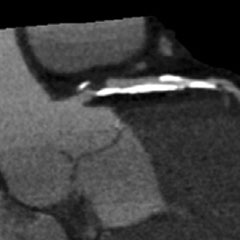 | 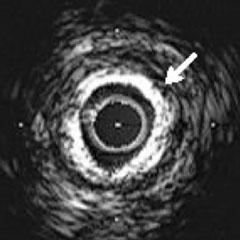 | 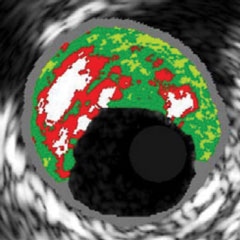 | 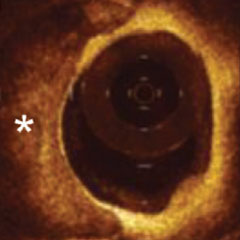 |
| Detection of coronary artery calcium | + | +++ | +++ | +++ | ++++ |
| Localization of coronary artery calcium | + | +++ | +++ | +++ | ++++ |
| Quantification of coronary artery calcium | + | +++ | ++ | +++ | ++++ |
 |  |  |  |  |
Successful PCI and reduction in future revascularizations are closely tied to final stent expansion.1 Coronary artery calcification is often underappreciated by angiography because angiography underestimates morphological lesion severity which impacts treatment strategy.5
Using OCT imaging with MLD MAX workflow to guide PCI helps to determine the right treatment approach and achieve optimal stent expansion. In LightLab, operators achieved 80% minimal stent expansion on average when following MLD MAX workflow.
References
- Shlofmitz, E., Sosa, F. A., Ali, Z. A., Waksman, R., Jeremias, A., & Shlofmitz, R. (2019). OCT-Guided Treatment of Calcified Coronary Artery Disease: Breaking the Barrier to Stent Expansion. Current Cardiovascular Imaging Reports, 12(8), 32.
- Dean Kereiakes, Disrupt CAD III: Lithotripsy for Vessel Preparation in Calcified Coronary Arteries Prior to Stenting, CLD. Dec 29, 2020.
- Madhavan MV, Tarigopula M, Mintz GS, Maehara A, Stone GW, Généreux P. Coronary artery calcification: pathogenesis and prognostic implications. J Am Coll Cardiol. 2014 May 06;63(17):1703-14.
- Räber L, et al. Clinical use of intracoronary imaging. Part 1: guidance and optimization of coronary interventions. An expert consensus document of the European Association of Percutaneous Cardiovascular Interventions. Eur Heart J. 2018;39(35):3281-3300.
- Croce, K. et al: Optical Coherence Tomography Influences Procedure and Vessel Preparation Decisions During Percutaneous Coronary Intervention – Insights from the LightLab Initiative. TCTConnect2020 Presentation.
- Fujino, A et al. A new optical coherence tomography-based calcium scoring system to predict stent underexpansion. EuroIntervention. 2018 Apr 6;13(18):e2182-e2189. doi: 10.4244/EIJ-D-17-00962.
- Wang, X et al. In vivo calcium detection by comparing optical coherence tomography, intravascular ultrasound, and angiography. JACC Cardiovasc Imaging. 2017 Aug;10(8):869-879. doi: 10.1016/j.jcmg.2017.05.014.
- Mintz,G. Intravascular Imaging of Coronary Calcification and its Clinical Implications. JACC Cardiovascular Imaging, 2015. https://dx.doi.org/10.1016/j.jcmg.2015.02.003
MAT-2105105 v2.0