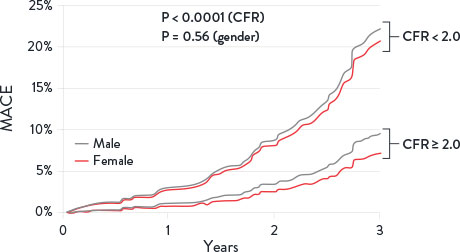
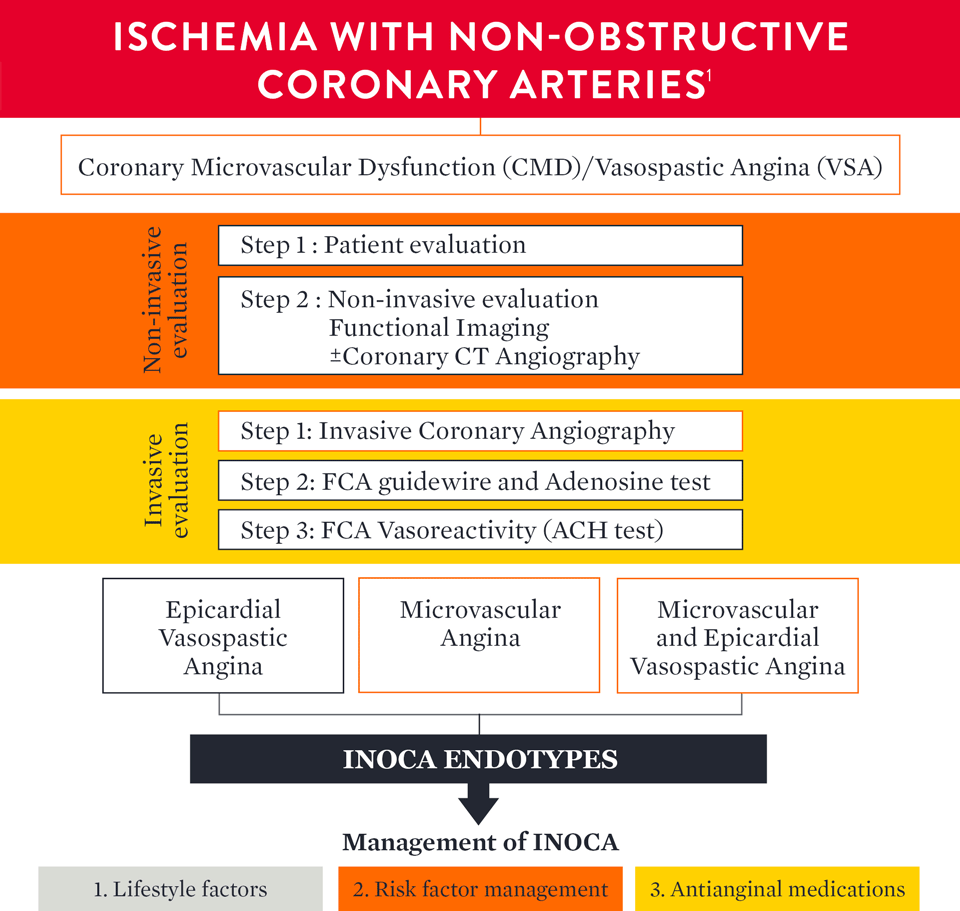
Angina is a condition that affects over 112 million people around the world.1 Many patients with angina undergo coronary angiography to assess the epicardial arteries and identify the root cause of angina.1 Unfortunately, angiography cannot assess the microcirculation—responsible for much of the regulation and distribution of blood flow to the myocardium.2 This means the majority (approximately 60%) of patients assessed for angina are found to have no angiographic abnormalities, but still have symptoms of a coronary disorder.3,4
Additionally, 20-30% of patients continue to experience persistent angina even after percutaneous coronary intervention (PCI), making repeat visits to the cardiologist’s office, where a lack of a clear diagnosis can make it difficult to determine a clear plan for disease management. These patients with ischemia and no obstructive coronary artery disease (INOCA) and/or post-PCI angina may be suffering from Coronary Microvascular Dysfunction (CMD),5 defined as impaired blood flow to the microcirculation.2
Hear Prof. Divaka Perera, a consultant cardiologist from London, UK, discuss why measuring microvascular function for CMD can improve patient management.
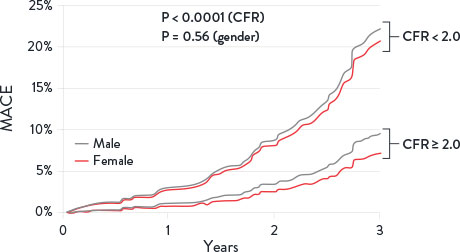
INOCA is not benign2 or a final diagnosis. Up to 50% of stable patients undergoing angiography have INOCA who may be suffering from CMD.4
Additionally, these patients have an increase in diastolic dysfunction and cardiac death2
CMD is defined by cardiac positron emission tomography/computed tomography CFR < 2 in patients without overt obstructive coronary artery disease.
MACE = Major Adverse Cardiovascular Events. Image adapted from Taqueti et al. J Am Cardiol. 2018²
MAT-2302514 v1.0

Indications: CoroFlow‡ is indicated to provide hemodynamic information for use in the diagnosis of patients with cardiovascular diseases.
CoroFlow‡ is intended for use in catheterization and related cardiovascular specialty laboratories to compute and display various physiological parameters based on the output from one or more measuring devices.
Contraindications: The system has no patient alarm functions. Do not use for cardiac/vital signs monitoring.
Warnings:
Precautions:
MAT-2007904 v3.0

Indications: The PressureWire™ X Guidewire is indicated to direct a catheter through a blood vessel and to measure physiological parameters in the heart and in the coronary and peripheral blood vessels. Physiological parameters include blood pressure. The PressureWire™ X Guidewire can also measure blood temperature.
Contraindications: This guidewire is contraindicated for use in the cerebral vasculature.
Warnings:
Precautions:
Potential Adverse Events: Potential complications which may be encountered during all catheterization procedures include, but are not limited to: vessel dissection or occlusion, perforation, embolus, spasm, local and/or systemic infection, pneumothorax, congestive heart failure, myocardial infarction, hypotension, chest pain, renal insufficiency, serious arrhythmias, or death.
In addition, this device has a coating containing Polyethylene Glycol (PEG); potential allergic reactions (anaphylaxis) may occur during the interventional procedure if the patient is allergic to PEG.
MAT-2103599 v2.0
Stay Connected