Explore Abbott's Portfolio of Self-Expanding and Balloon-Expanding Stents.
Self-Expanding Stents
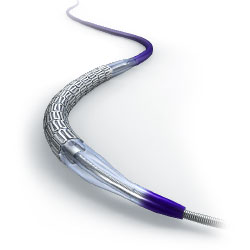
Supera™ Peripheral Stent System
- Interwoven wires that mimic the dynamic twisting, bending, and shortening of the SFA and proximal popliteal1
Absolute Pro™ Vascular Self-Expanding Stent System
- Tri-axial technology designed to ensure precise stent placement
Balloon-Expanding Stents
Omnilink Elite™ Vascular Balloon-Expandable Stent System
- Cobalt chromium multi-link technology that allows for thin struts without sacrificing strength for flexibility and vessel conformability
Herculink Elite™ Renal Stent System
- Excellent strength and deliverability to the renal arteries
Data on file at Abbott unless otherwise noted.
References
- Chan et al. Predictors of restenosis in the use of helical interwoven nitinol stents to treat femoropopliteal occlusive disease. Journal of Vascular Surgery; November 2015; 62:1201-9.
MAT-2114443 v1.0
Supera™ Peripheral Stent System

Indications
The Supera™ Peripheral Stent System is indicated to improve luminal diameter in the treatment of patients with symptomatic de novo or restenotic native lesions or occlusions of the superficial femoral artery (SFA) and / or proximal popliteal artery with reference vessel diameters of 4.0 to 7.5 mm, and lesion lengths up to 140 mm.
Contraindications
The Supera™ Peripheral Stent System is contraindicated in:
- Patients who are judged to have a lesion that prevents complete inflation of an angioplasty balloon or proper placement of the stent or stent delivery system.
- Patients who cannot receive antiplatelet or anticoagulation therapy. Based on in vivo thrombogenicity testing, the device should not be used in patients who cannot be anticoagulated as there may be some thrombus formation in the absence of anticoagulation.
Warnings
- This device is intended for single-use only. Do not reuse. Do not resterilize. Do not use if the package is opened or damaged.
- Use this device prior to the “Use By” date as specified on the device package label. Store in a dry, dark, cool place.
- DO NOT use if it is suspected that the sterility of the device has been compromised.
- Persons with known hypersensitivities to Nitinol and / or its components (e.g. nickel-titanium) may suffer an allergic reaction to this implant.
- Administer appropriate antiplatelet therapy pre- and post-procedure.
- Careful attention should be paid when sizing and deploying the stent to prevent stent elongation. In the SUPERB clinical study, stent elongation was associated with a decrease in patency at 12 months.
Precautions
The Supera™ Peripheral Stent System should only be used by physicians and medical personnel trained in vascular interventional techniques and trained on the use of this device.
- The long-term safety and effectiveness of the Supera™ Peripheral Stent System has not been established beyond three years.
- The safety and effectiveness of the Supera™ Peripheral Stent System has not been established in patients who:
- are less than 18 years old
- are pregnant or lactating
- have in-stent restenosis of the target lesion
- have known hypersensitivity to any component of the stent system (e.g., nickel)
- cannot tolerate contrast media and cannot be pre-treated
- have uncontrolled hypercoagulability and / or another coagulopathy
- This device is not designed for use with contrast media injection systems or power injection systems.
- The flexible design of the Supera™ stent may result in variation in the deployed stent length.
Magnetic Resonance Imaging (MRI) Safety Information
Nonclinical testing has demonstrated that the Supera™ stent, in single and in overlapped configurations up to 250 mm in length, is MR Conditional. A patient with this device can be safely scanned in an MR system meeting the following conditions:
- Static magnetic field of 1.5 or 3.0 Tesla
- Maximum spatial gradient magnetic field of 2,500 Gauss/cm (25 T/m)
- Maximum MR whole-body-averaged specific absorption rate (SAR) of
- 2 W/kg for landmarks (i.e. center of RF coil) above the umbilicus
- 1 W/kg for landmarks below the umbilicus and above the mid-thigh
- 0.5 W/kg for landmarks below the mid-thigh
Under the scan conditions defined above, the Supera™ stent is expected to produce a maximum temperature rise of 7.6 °C after 15 minutes of continuous scanning.
In nonclinical testing, the image artifact caused by the device extends approximately 2 cm from the Supera™ stent when imaged with a gradient echo or spin echo sequence and a 3T MRI system.
Potential Adverse Events
Potential adverse events include, but are not limited to:
- Abrupt closure
- Allergic reaction (contrast medium; drug; stent material)
- Amputation or limb loss
- Aneurysm or pseudoaneurysm in vessel or at vascular access site
- Angina or coronary ischemia
- Arrhythmia (including premature beats, bradycardia, atrial or ventricular tachycardia, atrial or ventricular fibrillation)
- Arteriovenous fistula
- Bleeding complications requiring transfusion or surgical intervention
- Death
- Detachment of a system component or implantation in an unintended site
- Embolization, arterial or other (e.g. air, tissue, plaque, thrombotic material, or stent)
- Emergent surgery
- Fever
- Hematoma or hemorrhagic event, with or without surgical repair
- Hyperperfusion syndrome
- Hypertension / Hypotension
- Infection
- Myocardial infarction
- Pain (leg, foot, and/or insertion site)
- Partial stent deployment
- Peripheral nerve injury
- Pulmonary embolism
- Renal failure or insufficiency
- Restenosis of vessel in stented segment
- Shock
- Stent malapposition or migration, which may require emergency surgery to remove stent
- Stent strut fracture
- Thrombosis or occlusion
- Stroke
- Transient ischemic attack
- Venous thromboembolism
- Vessel dissection, perforation or rupture
- Vessel spasm or recoil
- Worsening claudication or rest pain
MAT-2103597 v3.0
Absolute Pro™
Vascular Self-Expanding Stent System

Indications
The Absolute Pro™ Vascular Self-Expanding Stent System is indicated for improving luminal diameter in patients with de novo or restenotic atherosclerotic lesions in the native common iliac artery and native external iliac artery with reference vessel diameters between 4.3 mm to 9.1 mm and lesion lengths up to 90 mm.
Contraindications
There are no known contraindications.
Warnings
DO NOT USE IF THE TEMPERATURE INDICATOR IS BLACK.
This device is intended for single-use only; do not reuse. Do not resterilize. Do not use if the package is open or damaged.
Use prior to the “Use By” date specified on the package.
Persons with known hypersensitivities to nitinol and / or its components (e.g. nickel, titanium) may suffer an allergic reaction to this implant.
The safety and effectiveness of multiple overlapping stents have not been established. However, when multiple stents are required, stent materials should be of similar composition.
Stenting across a major bifurcation may hinder or prevent future diagnostic or therapeutic procedures.
Use of an undersized guide wire, with insufficient support, may cause kinking in the Stent Delivery System.
Use of appropriate anticoagulant and/or antiplatelet therapy per standard of care is recommended for use with this stent system.
Precautions
- Inspect the product prior to use. Do not use if the package is open or damaged. Avoid unnecessary handling, which may kink or damage the Delivery System.
- Only physicians familiar with the complications, side effects and hazards commonly associated with iliac stent placement should use this device.
- The stent is not designed for resheathing or recapturing. The stent is not designed for repositioning once the stent has apposed the vessel wall.
- Once the stent is apposed to the vessel, it is not recommended to remove the stent with the delivery system.
- The Absolute Pro™ is intended to perform as a system. Do not remove the stent for use in conjunction with other dilatation catheters; do not use the Absolute Pro in conjunction with other stents.
- Refer to the instructions for use supplied with any interventional devices to be used in conjunction with the Absolute Pro for their intended uses, contraindications, and potential complications.
- Stent retrieval methods (use of additional wires, snares and / or forceps) may result in additional trauma to the vasculature.
Stent Delivery System Handling – Precautions
- Do not remove the stent from its Delivery System, as removal may damage the stent and / or lead to stent embolization. Stent system is intended to perform as a system.
- Special care must be taken not to handle or in any way disrupt the stent on the Delivery System. This is most important during Delivery System removal from packaging, mandrel removal, placement over guide wire, and advancement through rotating hemostatic valve (RHV) adapter and guiding catheter hub.
- Inspect to determine the outer jacket is attached to the handle. Reattach by pushing the outer jacket back into the handle.
- If the thumbwheel moves prior to unlocking, do not use unit; unintentional partial or full deployment may occur.
- Do not unlock the handle prior to positioning the stent at the intended location. Failure to follow this instruction could lead to deployment of the stent at an unintended location.
- Once unlocked, the handle locking mechanism cannot be re-locked.
- Once unlocked, the retraction sheath may unintentionally release the stent during device manipulation.
Stent Placement - Precautions
- Advance the Delivery System past the lesion and pull back to help remove slack from the system. Removing all slack from the delivery system prior to stent deployment will help ensure accurate stent delivery.
- If detachable outer jacket is not engaged in the introducer sheath, manually stabilize prior to deployment to help ensure accurate stent delivery. Do not restrict retracting sheath during stent deployment.
- If the thumbwheel moves freely in both directions after unlocking, remove the device together with the introducer sheath or guiding catheter as single unit; do not use the unit as unintentional partial or full deployment may occur.
- Do not attempt to pull a partially expanded stent back through the sheath or guiding catheter; dislodgment of the stent from the Delivery System may occur.
- Should unusual resistance be felt at any time, including resistance unlocking the handle or rotating the thumbwheel, during stent deployment, the entire system should be removed together with the introducer sheath or guiding catheter as a single unit. Failure to follow these instructions could result in failure to deploy, difficulties with deployment, partial stent deployment or deployment in an unintended location.
- Do not expand the stent if it is not properly positioned in the vessel. (See Stent / System Removal – Precautions.)
Stent / System Removal – Precautions
Do not attempt to pull a partially-expanded stent back through the introducer sheath or guiding catheter. The stent is not designed for recapturing. The stent is not designed for repositioning once the stent has apposed the vessel. Once the stent is apposed to the vessel, it is not recommended to remove the stent with the Delivery System.
Should unusual resistance be felt at any time during lesion access or removal of the Delivery System post stent implantation, the entire system should be removed together with the introducer sheath or guiding catheter as a single unit. Failure to follow these instructions could result in failure to deploy, difficulties with deployment, partial stent deployment or deployment in an unintended location.
When removing the Delivery System as a single unit:
- Do not retract the Delivery System into the guiding catheter or sheath.
- Tighten the RHV (if applicable) to secure the Delivery System to the guiding catheter, and then remove the guiding catheter or sheath and Delivery System as a single unit.
- If possible, retain the guide wire position for subsequent vessel access.
Failure to follow these steps and / or applying excessive force to the Delivery System can potentially result in loss or damage to the stent and / or Delivery System components.
Post Implant – Precautions
- Exercise great care when crossing a newly deployed stent with a guide wire, balloon or Delivery System to avoid disrupting the stent geometry.
- This stent is an open cell design. Open cell designs allow each ring to expand independently of the adjacent ring. Under fluoroscopy the independent ring expansion may appear as a step in the contour of the stent, and be erroneously interpreted as a stent fracture. This should be considered when deciding whether additional diagnostics (x-ray and / or angiography with contrast material) is necessary.
Magnetic Resonance Imaging (MRI)
Non-clinical testing has demonstrated that the Absolute Pro Stent in single and in overlapped configurations up to 190 mm in length is MR Conditional as defined in ASTM F2503. For placement in the iliac artery, patients with this implant may be scanned safely anytime after implantation under the following conditions:
- Static magnetic field of 1.5 Tesla or 3.0 Tesla.
- Spatial gradient field of 2500 Gauss/cm or less.
- Maximum whole body average specific absorption rate (WB-SAR) of 2 W/kg for 15 minutes of scanning per sequence for patient landmarks above umbilicus. (Total duration of all scans may exceed 15 minutes.)
- Maximum WB-SAR of 1W/kg for 15 minutes of scanning for patient landmarks below umbilicus.
- Transmit RF body coil should be used in normal operating mode, as defined in IEC 60601-2-33.
The Absolute Pro™ stent should not migrate in this MRI environment. Magnetic force on the Absolute Pro stent was tested according to ASTM F2052-06e. Non-clinical testing at field strengths greater than 3 Tesla has not been performed to evaluate stent migration or heating.
Stent heating during MRI was derived by using the measured non-clinical, in vitro temperature rise according to ASTM F2182-09 in a GE Signa HDx 3 Tesla scanner and in a GE 1.5 Tesla coil in combination with the calculated local specific absorption rates (SARs) in a digitized human model. For the SAR conditions above, the greatest in-vivo temperature rise was calculated to be 5.3°C at 128 MHz for a stent length of 60 mm. The calculations do not take into consideration the cooling effects of blood flow, and therefore, actual in-vivo rises are expected to be lower.
The effects of MRI on overlapped stents greater than 190 mm in length or stents with fractured struts are unknown. Image artifact may be present when scanning the Absolute Pro stent as demonstrated in non-clinical testing performed according to ASTM F2119-07 in a GE Signa HDx 3 Tesla scanner. The image artifact (both inside and outside the device lumen) extends approximately 5 mm from the device using the spin echo sequence and 10 mm from the device using the gradient echo sequence. MR image quality may be compromised if the area of interest is in the exact same area, or relatively close to, the position of the Absolute Pro stent. Therefore, it may be necessary to optimize the MR imaging parameters in the presence of Absolute Pro stents.
Abbott Vascular recommends that patients register the MR conditions in this IFU with the MedicAlert Foundation or equivalent organization. The MedicAlert Foundation can be contacted by phone at: (888) 633-4298, (209) 668-3333 or on the internet at www.medicalert.org.
Potential Adverse Events
Below is a list of the potential adverse effects (e.g., complications) that may be associated with the use of the device:
- Acute myocardial infarction
- Allergic reaction (contrast medium, drug or stent material)
- Aneurysm, pseudoaneurysm, or arteriovenous fistula
- Angina or coronary ischemia
- Arrhythmias, with or without the need for a temporary pacemaker
- Bleeding complications from anticoagulant or antiplatelet medication requiring transfusion or surgical intervention
- Death
- Detachment and/or implantation of a component of the system
- Embolization, arterial or other (air, tissue, plaque, thrombotic material, stent)
- Emergent or urgent surgery to perfuse limb or remove stent
- Fever
- Hematoma or hemorrhagic event
- Hypotension or hypertension
- Infection, local or systematic, including bacteremia or septicemia
- Ischemia or infarction of tissue or organ
- Pain (limb or catheter insertion site)
- Pulmonary embolism
- Renal failure or insufficiency secondary to contrast medium
- Restenosis of vessel in stented segment
- Stent malapposition or migration
- Stent strut fracture
- Stent thrombosis or occlusion
- Stroke, cerebrovascular accident (CVA), or transient ischemic attack (TIA)
- Target limb loss (amputation of toe, foot, and/or leg)
- Vascular thrombosis or occlusion at puncture site, treatment site, or remote site
- Vessel dissection, perforation, or rupture
- Vessel spasm or recoil
- Worsening claudication or rest pain
MAT-2114529 v2.0
Omnilink Elite™
Vascular Balloon-Expandable Stent System

INDICATIONS
The Omnilink Elite™ Stent System is indicated for the treatment of atherosclerotic iliac artery lesions with reference vessel diameters of ≥ 5.0 mm and ≤ 11.0 mm, and lesion lengths up to 50 mm.
CONTRAINDICATIONS
There are no known contraindications.
WARNINGS
- This device is intended for single-use only; do not reuse. Do not resterilize. Do not use if package is open or damaged.
- Since the use of this device carries the associated risk of subacute thrombosis, vascular complications, and / or bleeding events, judicious selection of patients is necessary.
- Persons allergic to L605 cobalt chromium alloy may suffer an allergic reaction to this implant.
- This device should be used only by physicians trained in angiography and percutaneous transluminal angioplasty and stent placement.
- The safety and effectiveness of multiple overlapping stents have not been established. However, when multiple stents are required, stent materials should be of similar composition to avoid the potential for dissimilar metal corrosion.
- Use of appropriate anticoagulant and / or antiplatelet therapy per standard of care is recommended for use with this stent system.
PRECAUTIONS
The device should be used only by physicians trained in angiography and percutaneous transluminal angioplasty and stent placement.
Stent Delivery System Handling – Precautions
- For single use only. Do not resterilize or reuse.
- Use the stent system prior to the “Use by” date specified on the package.
- Do not remove stent from its delivery balloon, as removal may damage the stent and / or lead to stent embolization.
- Carefully inspect the Omnilink Elite™ Stent System prior to use to verify that the stent has not been damaged in shipment and that the device dimensions are suitable for the specific procedure. Take care to avoid unnecessary handling.
- The Omnilink Elite™ Stent System is intended to perform as a system. The stent should not be removed for use in conjunction with other dilatation catheters, nor should the delivery system be used in conjunction with other stents.
- Refer to the instructions for use supplied with any interventional devices to be used in conjunction with the Omnilink Elite™ Stent System, for their intended uses, contraindications, and potential complications.
- Special care must be taken not to handle or in any way disrupt the stent on the balloon. This is most important during stent system removal from the packaging, placement over a guide wire and advancement through a guiding catheter or introducer sheath.
- Do not "roll" the mounted stent with your fingers, as this action may loosen the stent from the delivery balloon.
- Use only the appropriate balloon inflation media. Do not use air or any gaseous medium to inflate the balloon, as this may cause uneven expansion and difficulty in deployment of the stent.
- Do not advance the stent delivery system without the guide wire extending from the tip.
Stent Placement – Precautions
- Do not prepare or pre-inflate balloon prior to stent deployment other than as directed. Use balloon purging technique described in the Clinician Use Information section.
- The inflated balloon diameter of the system used to deploy the stent should approximate the diameter of the vessel. Oversizing of the stent can result in a ruptured vessel. To ensure full expansion of the stent, the balloon should be inflated to a minimum of nominal pressure.
- Implanting a stent may lead to dissection of the vessel distal and / or proximal to the stent and may cause acute closure of the vessel, requiring additional intervention (surgical intervention, further dilatation, placement of additional stents, or other).
- When treating multiple lesions, the distal lesion should be initially stented, followed by stenting of the proximal lesion. Stenting in this order obviates the need to cross the proximal stent in placement of the distal stent and reduces the chances for dislodging the proximal stent.
- Do not expand the stent if it is not properly positioned in the vessel (see Stent / System Removal – Precautions).
- Stenting across a major bifurcation may hinder or prevent future side branch access.
- Balloon pressures should be monitored during inflation. Do not exceed Rated Burst Pressure (RBP) as indicated on product label. Use of pressures higher than specified on product label may result in a ruptured balloon with possible vessel damage or perforation.
- Stent retrieval methods (use of additional wires, snares, and / or forceps) may result in additional trauma to the vasculature and / or the vascular access site. Complications may include bleeding, hematoma, or pseudoaneurysm.
- The Omnilink Elite™ Stent System is intended for deployment and post-deployment dilatation of the stent only and should not be used to dilate other locations.
- Do not attempt to pull an unexpanded stent back through the introducer sheath / guiding catheter; dislodgment of the stent from the balloon may occur.
- Once fully deployed, the stent cannot be repositioned.
Stent / System Removal – Precautions
Should unusual resistance be felt at any time during either lesion access or removal of the delivery system post-stent implantation, the entire system should be removed as a single unit.
When removing the delivery system as a single unit:
- DO NOT retract the delivery system into the introducer sheath / guiding catheter.
- Position the proximal balloon marker just distal to the tip of the introducer sheath / guiding catheter.
- Advance the guide wire in the anatomy as far distally as safely possible.
- Secure the delivery system to the introducer sheath / guiding catheter; then remove the introducer sheath / guiding catheter, guide wire and delivery system as a single unit.
Failure to follow these steps and / or applying excessive force to the delivery system can potentially result in loss or damage to the stent and / or delivery system components. If it is necessary to retain guide wire position for subsequent vessel access, leave the guide wire in place and remove all other system components.
Post Implant – Precautions
Exercise great care when crossing a newly deployed stent with a guide wire or balloon catheter to avoid disrupting the stent geometry.
Magnetic Resonance Imaging (MRI) Information
Non-clinical testing has demonstrated that the Omnilink Elite™ stent, in single and in overlapped configurations up to 100 mm in length, is MR Conditional as defined in ASTM F2503. It can be scanned safely under the conditions listed in the Instructions for Use.
POTENTIAL ADVERSE EVENTS
Potential complications associated with percutaneous iliac artery treatment, including the use of an iliac stent, may include, but are not limited to, the following:
- Acute myocardial infarction
- Allergic reaction (contrast medium, drug, or stent material)
- Aneurysm, pseudoaneurysm, or arteriovenous fistula
- Angina or coronary ischemia
- Arrhythmias, with or without the need for a temporary pacemaker
- Bleeding complications from anticoagulant or antiplatelet medication requiring transfusion or surgical intervention
- Death
- Detachment and / or implantation of a component of the system
- Embolization, arterial or other (air, tissue, plaque, thrombotic material, stent)
- Emergent or urgent surgery to perfuse limb or remove stent
- Fever
- Hematoma or hemorrhagic event
- Hypotension or hypertension
- Infection, local or systemic, including bacteremia or septicemia
- Ischemia or infarction of tissue or organ
- Pain (limb or catheter site)
- Pulmonary embolism
- Renal failure or insufficiency secondary to contrast medium
- Restenosis of vessel in stented segment
- Stent malapposition or migration
- Stent strut fracture
- Stent thrombosis or occlusion
- Stroke, cerebrovascular accident (CVA), or transient ischemic attack (TIA)
- Target limb loss (amputation of toe, foot, and / or leg)
- Vascular thrombosis or occlusion at puncture site, treatment site, or remote site
- Vessel dissection, perforation, or rupture
- Vessel spasm or recoil
- Worsening claudication or rest pain
MAT-2114535 v2.0
Herculink Elite™
Renal Stent System

Indications
The RX Herculink Elite™ Renal Stent System is indicated for use in patients with atherosclerotic disease of the renal arteries following sub-optimal percutaneous transluminal renal angioplasty (PTRA) of a de novo or restenotic atherosclerotic lesion (≤ 15 mm in length) located within 10 mm of the renal ostium and with a reference vessel diameter of 4.0 - 7.0 mm. Suboptimal PTRA is defined as ≥ 50% residual stenosis, ≥ 20 mmHg peak systolic or ≥ 10 mmHg mean translesional pressure gradient, flow-limiting dissection, or TIMI [Thrombolysis In Myocardial Infarction] flow < 3.
Contraindications
The RX Herculink Elite™ Renal Stent System is contraindicated for use in:
- Patients with a contraindication for antiplatelet/ anticoagulant therapy Patients who have a lesion that cannot be crossed with a wire or a balloon angioplasty catheter
- Patients with bleeding disorders
- Patients with a known hypersensitivity to cobalt or chrome
- Target lesions that are resistant to complete balloon inflation
- Stenting of an arterial vessel where leakage from the artery could be exacerbated by placement of a stent
- Patients with a target lesion with a large amount of adjacent acute or subacute thrombus.
Warnings
The long term safety and effectiveness of this device for use in the renal arterial system have not been established.
Should unusual resistance be felt at any time during lesion access or Delivery System removal, the introducer sheath/guiding catheter and stent system should be removed as a single unit. Applying excessive force to the Stent Delivery System can potentially result in loss or damage to the Stent and Delivery System components. (See Stent/System Removal – Precautions.)
Since the use of this device carries the associated risk of subacute thrombosis, vascular complications and/or bleeding events, judicious selection of patients is necessary.
Stenting across a major bifurcation may hinder or prevent future diagnostic or therapeutic procedures.
Once fully deployed, the stent cannot be repositioned.
Persons allergic to L605 cobalt chromium alloy may suffer an allergic reaction to this implant.
Only physicians familiar with the complications, side effects and hazards commonly associated with renal stent placement should use this device.
The RX Herculink Elite™ Renal Stent System is intended to perform as a system. The stent should not be removed for use in conjunction with other dilatation catheters, nor should the RX Herculink Elite™ Renal Stent System be used in conjunction with other stents.
The safety and effectiveness of multiple overlapping stents have not been established. However, when multiple stents are required, stent materials should be of similar composition.
Precautions
Stent Delivery System Handling – Precautions
- For single use only. Do not resterilize or reuse. Note product “Use By” date. Do not remove stent from its delivery balloon as removal may damage the stent and/or lead to stent embolization.
- Carefully inspect the RX Herculink Elite™ Renal Stent System prior to use to verify that the stent has not been damaged in shipment and that the device dimensions are suitable for the specific procedure. Take care to avoid unnecessary handling.
- Refer to the instructions for use supplied with any interventional devices to be used in conjunction with the RX Herculink Elite™ Renal Stent System, for their intended uses, contraindications, and potential complications.
- Special care must be taken not to handle or in any way disrupt the stent on the balloon. This is most important during stent system removal from the packaging, placement over a guide wire and advancement through a guiding catheter or introducer sheath.
- Do not “roll” the mounted stent with your fingers as this action may loosen the stent from the delivery balloon.
- Use only the appropriate balloon inflation media. Do not use air or any gaseous medium to inflate the balloon as this may cause uneven expansion and difficulty in deployment of the stent.
Stent Placement - Precautions
- Do not prepare or pre-inflate balloon prior to stent deployment other than as directed.
- Use balloon purging technique described in the ‘Clinician Use Information’ section.
- The inflated balloon diameter of the system used to deploy the stent should approximate the diameter of the vessel. Oversizing of the stent can result in a ruptured vessel. To ensure full expansion of the stent, the balloon should be inflated to a minimum of nominal pressure.
- Implanting a stent may lead to dissection of the vessel distal and/or proximal to the stent and may cause acute closure of the vessel requiring additional intervention (surgical intervention, further dilatation, placement of additional stents, or other).
- Do not expand the stent if it is not properly positioned in the vessel. (See Stent/System Removal - Precautions.)
- Stenting across a major bifurcation may hinder or prevent future side branch access.
- Balloon pressures should be monitored during inflation. Do not exceed Rated Burst Pressure (RBP) as indicated on product label. Use of pressures higher than specified on product label may result in a ruptured balloon with possible vessel damage or perforation.
- Stent retrieval methods (use of additional wires, snares and/or forceps) may result in additional trauma to the vasculature and/or the vascular access site. Complications may include bleeding, hematoma or pseudoaneurysm.
- The RX Herculink Elite™ Renal Stent System is intended for deployment and post-deployment dilatation of the stent only and should not be used to dilate other lesions.
- Do not attempt to pull an unexpanded stent back through the introducer sheath/guiding catheter; dislodgment of the stent from the balloon may occur.
Stent / System Removal – Precautions
Should unusual resistance be felt at any time during either lesion access or removal of the Delivery System post-stent implantation, the entire system should be removed as a single unit.
When removing the Delivery System as a single unit:
- DO NOT retract the Delivery System into the introducer sheath/guiding catheter.
- Position the proximal balloon marker just distal to the tip of the introducer sheath/guiding catheter.
- Advance the guide wire in the anatomy as far distally as safely possible.
- Secure the Delivery System to the introducer sheath/guiding catheter; then remove the introducer sheath/guiding catheter, guide wire and Delivery System as a single unit.
Failure to follow these steps and / or applying excessive force to the Delivery System can potentially result in loss or damage to the stent and / or delivery system components.
If it is necessary to retain guide wire position for subsequent vessel access, leave the guide wire in place and remove all other system components.
Post Implant – Precautions
Great care must be exercised when crossing a newly deployed stent with a guide wire or balloon catheter to avoid disrupting the stent geometry.
Magnetic Resonance Imaging (MRI): Non-clinical testing has demonstrated that the Herculink Elite™ stent, in single and in overlapped configurations up to 33 mm in length, is MR Conditional. It can be scanned safely under the following conditions:
- Static magnetic field of 1.5 or 3 Tesla
- Spatial gradient field of 2500 Gauss/cm or less
- Maximum whole-body-averaged specific absorption rate (SAR) of 2.0 W/kg (normal operating mode) for any duration of MRI scan that would otherwise be safe for the patient without implant.
MRI at 1.5 or 3 Tesla may be performed immediately following the implantation of the Herculink Elite™ stent.
The Herculink Elite™ stent should not migrate in this MRI environment. Magnetic force on the Herculink Elite™ stent was tested according to ASTM F2052-06e. Non-clinical testing at field strengths greater than 3 Tesla has not been performed to evaluate stent migration or heating.
Stent heating was derived by using the measured non-clinical, in vitro temperature rise according to ASTM F2182-09 in a GE Signa HDx 3 Tesla scanner and in a GE 1.5 Tesla coil in combination with the local specific absorption rates (SARs) in a digitized human heart model. The temperature rise was derived by a validated calculation. At overlapped lengths up to 33 mm, the Herculink Elite™ stent produced a non-clinical maximum local temperature rise of less than 3ºC at a maximum whole body averaged SAR of 2.0 W/kg (normal operating mode) for an MRI sequence of 15 minutes. These calculations do not take into consideration the cooling effects of blood flow.
The effects of MRI on overlapped stents greater than 33 mm in length or stents with fractured struts are unknown.
Image artifact may be present when scanning the Herculink Elite™ stent as demonstrated in non-clinical testing performed according to ASTM F2119-07 in a GE Signa HDx 3 Tesla scanner. The image artifact (both inside and outside the device lumen) extends approximately 7 mm from the device using the spin echo sequence (TR = 500 ms; TE = 20 ms; flip angle = 90°) and 13 mm from the device using the gradient echo sequence (TR = 100 ms; TE = 15 ms; flip angle = 30°). MR image quality may be compromised if the area of interest is in the exact same area, or relatively close to, the position of the Herculink Elite™ stent. Therefore, it may be necessary to optimize the MR imaging parameters in the presence of Herculink Elite™ stents.
Potential Adverse Events
Potential complications associated with percutaneous renal artery treatment including the use of a renal stent may include, but are not limited to, the following:
- Abscess
- Allergic reaction to Cobalt Chromium or contrast agents
- Arrhythmias (ventricular fibrillation, ventricular tachycardia, other)
- Arteriovenous fistula
- Bowel infarct
- Death
- Dialysis
- Dissection
- Drug reaction to antiplatelet agents
- Drug reaction, allergic reaction to contrast media
- Emboli (air, tissue, or thrombotic emboli) resulting in tissue ischemia/infarction
- Emergency surgery to correct vascular complications
- Emergent renal artery bypass surgery
- Extremity ischemia/amputation
- Fever
- Gastrointestinal symptoms from anticoagulation/antiplatelet medication
- Hematoma at vascular access site
- Hemorrhage requiring transfusion
- Hypersensitivity reactions
- Hypertension / hypotension
- Infection and pain at vascular access site
- Intimal tear
- Kidney infarct
- Myocardial infarction
- Myocardial ischemia
- Nephrectomy
- Peripheral neuropathy
- Pseudoaneurysm at vascular access site
- Pseudoaneurysm formation
- Renal artery thrombosis, aneurysm, rupture, perforation, occlusion, spasm, or restenosis
- Renal insufficiency or failure
- Stent migration or embolization
- Stent misplacement
- Stroke/cerebral vascular accident
- Tissue necrosis or ulceration
MAT-2114538 v1.0