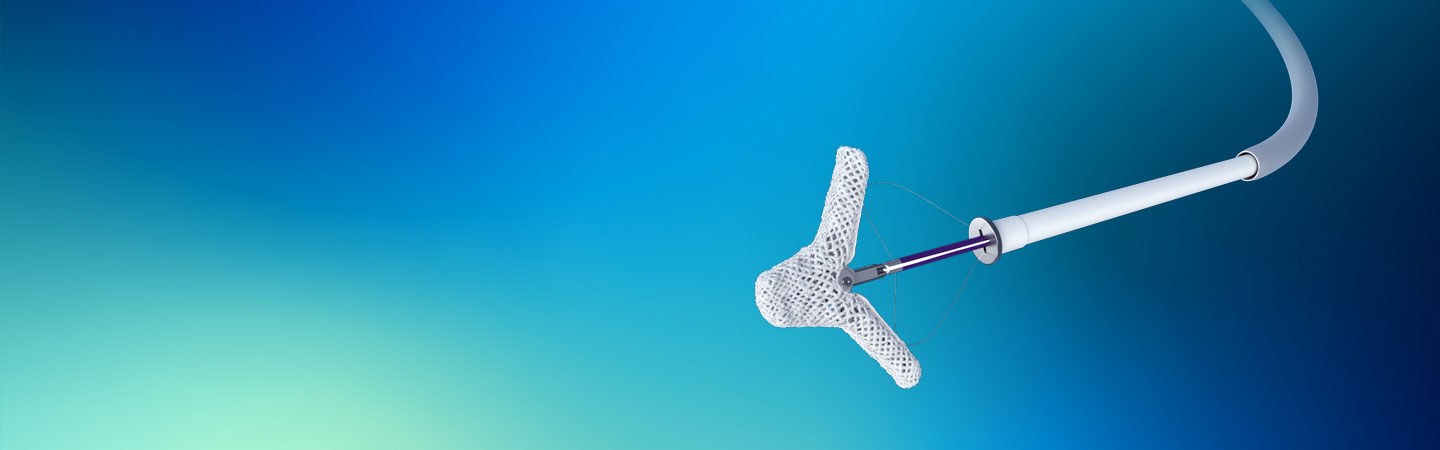
The Standard of Caring for TR
The TriClip™ G5 System offers a minimally invasive treatment option for improving quality of life and functional status in patients with symptomatic severe tricuspid regurgitation, despite optimal medical therapy, who are at intermediate or greater risk for surgery and in whom transcatheter edge-to-edge valve repair is clinically appropriate.
2020 AHA/ACC Guidelines Recommend Treatment of Severe TR
2020 AHA/ACC Guidelines recognize that severe tricuspid regurgitation (TR) may not improve predictably after treatment of the left-sided valve lesion and acknowledge that reoperation for severe, isolated TR after left-side valve treatment may be necessary.1
Learn more about TriClip TEER by visiting the Abbott Structural Heart website.
Ordering Information
TriClip G5 TEER System
| Product Code | Description | Piece Count |
|---|---|---|
| TCG50100 | TriClip G5 System | 1 |
| TCDS0801-NT | TriClip G5 NT Delivery System | 1 |
| TCDS0801-NTW | TriClip G5 NTW Delivery System | 1 |
| TCDS0801-XT | TriClip G5 XT Delivery System | 1 |
| TCDS0801-XTW | TriClip G5 XTW Delivery System | 1 |
| TSGC0801 | TriClip G5 Steerable Guide Catheter | 1 |
TriClip G5 Required Accessories
| Product Code | Description | Piece Count |
|---|---|---|
| SZR08 | Stabilizer | 1 |
| LFT07 | Lift | 1 |
| PLT07 | Support Plate | 1 |
TriClip G4 TEER System
| Product Code | Description | Piece Count |
|---|---|---|
| TCG40100 | TriClip G4 System | 1 |
| TCDS0301-NT | TriClip G4 NT Delivery System | 1 |
| TCDS0301-NTW | TriClip G4 NTW Delivery System | 1 |
| TCDS0301-XT | TriClip G4 XT Delivery System | 1 |
| TCDS0301-XTW | TriClip G4 XTW Delivery System | 1 |
| TSGC0201 | TriClip G4 Steerable Guide Catheter | 1 |
TriClip G4 Required Accessories - Other Countries (excluding U.S.)
| Product Code | Description | Piece Count |
|---|---|---|
| SZR07 | Stabilizer | 1 |
| LFT07 | Lift | 1 |
| PLT07 | Support Plate | 1 |
Europe, Middle East, and Africa
TriClip G4 System - EU MDR
| Product Code | Description | Piece Count |
|---|---|---|
| TC0307-NT | TriClip GT NT bundle [Content: one (1) TCDS0307-NT, one (1) TSGC0207] | 2 |
| TC0307-NTW | TriClip G4 NTW bundle (Contents: one (1) TCDS0307-NTW, one (1) TSGC0207] | 2 |
| TC0307-XT | TriClip G4 XT bundle [Contents: one(1) TCDS0307-XT, one (1) TSGC0207] | 2 |
| TC0307-XTW | TriClip G4 XTW bundle [Contents: one (1) TCDS0307-XTW, one (1) TSGC0207] | 2 |
| TCDS0307-NT | TriClip G4 NT Delivery System | 1 |
| TCDS0307-NTW | TriClip G4 NTW Clip Delivery System | 1 |
| TCDS0307-XT | TriClip G4 XT Delivery System | 1 |
| TCDS0307-XTW | TriClip G4 XTW Delivery System | 1 |
| TSGC0207 | TriClip Steerable Guide Catheter | 1 |
Required Accessories
| Product Code | Description | Piece Count |
|---|---|---|
| SZR07 | Stabilizer | 1 |
| LFT07 | Lift | 1 |
| PLT07 | Support Plate | 1 |

References
- Otto CM, Nishimura RA, Bonow RO, Carabello BA, Erwin JP 3rd, Gentile F, Jneid H, Krieger EV, Mack M, McLeod C, O’Gara PT, Rigolin VH, Sundt TM 3rd, Thompson A, Toly C. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2021;143:e72-e227. https://www.ahajournals.org/doi/10.1161/CIR.0000000000000923
MAT-2513222 v2.0
Rx Only
Important Safety Information
TRICLIP™ CLIP G5 SYSTEM
INDICATIONS
The TriClip™ G5 System is indicated for improving quality of life and functional status in patients with symptomatic severe tricuspid regurgitation despite optimal medical therapy, who are at intermediate or greater risk for surgery and in whom transcatheter edge-to-edge valve repair is clinically appropriate and is expected to reduce tricuspid regurgitation severity to moderate or less, as determined by a multidisciplinary heart team.
CONTRAINDICATIONS
The TriClip™ G5 System is contraindicated for use in patients with the following conditions: Intolerance, including allergy or untreatable hypersensitivity, to procedural anticoagulation; Untreatable hypersensitivity to Implant components (nickel-titanium alloy, cobalt-chromium alloy); Active endocarditis or other active infection of the tricuspid valve.
POTENTIAL ADVERSE EVENTS
The following events have been identified as possible complications of the TriClip™ G5 Procedure. Allergic reactions or hypersensitivity to latex, contrast agent, anaesthesia, device materials and drug reactions to anticoagulation, or antiplatelet drugs; Additional treatment / surgery from device-related complications; Bleeding; Blood disorders (including coagulopathy, hemolysis, and Heparin Induced Thrombocytopenia (HIT)); Cardiac arrhythmias (including conduction disorders, atrial arrhythmias, ventricular arrhythmias); Cardiac ischemic conditions (including myocardial infarction, myocardial ischemia, unstable angina, and stable angina); Cardiac perforation; Cardiac tamponade; Chest pain; Death; Dyspnea; Edema; Embolization (device or components of the device); Endocarditis; Fever or hyperthermia; Fluoroscopy and Transesophageal echocardiogram (TEE) -related complications: Skin injury or tissue changes due to exposure to ionizing radiation, Esophageal irritation, Esophageal perforation, Gastrointestinal bleeding; Hypotension / hypertension; Infection including: Septicemia; Nausea or vomiting; Pain; Pericardial effusion; Stroke / cerebrovascular accident (CVA) and transient ischemic attack (TIA); System organ failure: Cardio-respiratory arrest, Worsening heart failure, Pulmonary congestion, Respiratory dysfunction or failure or atelectasis, Renal insufficiency or failure, Shock (including cardiogenic and anaphylactic); Thrombosis; Tricuspid valve complications, which may complicate or prevent later surgical repair, including: Chordal entanglement / rupture, Single leaflet device attachment (SLDA), Dislodgement of previously implanted devices, Tissue damage, Tricuspid valve stenosis, Worsening, persistent or residual regurgitation; Vascular access complications which may require additional intervention, including: Wound dehiscence, Bleeding of the access site, Arteriovenous fistula, pseudoaneurysm, aneurysm, dissection, perforation (rupture), vascular occlusion, Embolism (air, thrombus), Peripheral nerve injury; Venous thrombosis (including deep vein thrombosis) and thromboembolism (including pulmonary embolism).
Rx Only
Important Safety Information
TRICLIP™ CLIP G4 SYSTEM
INDICATIONS
The TriClip™ G4 System is indicated for improving quality of life and functional status in patients with symptomatic severe tricuspid regurgitation despite optimal medical therapy, who are at intermediate or greater risk for surgery and in whom transcatheter edge-to-edge valve repair is clinically appropriate and is expected to reduce tricuspid regurgitation severity to moderate or less, as determined by a multidisciplinary heart team.
CONTRAINDICATIONS
The TriClip G4 System is contraindicated in patients with the following conditions: Intolerance, including allergy or untreatable hypersensitivity, to procedural anticoagulation; Untreatable hypersensitivity to Implant components (nickel-titanium alloy, cobalt-chromium alloy); Active endocarditis or other active infection of the tricuspid valve.
POTENTIAL ADVERSE EVENTS
The following events have been identified as possible complications of the TriClip G4 Procedure. Allergic reactions or hypersensitivity to latex, contrast agent, anaesthesia, device materials and drug reactions to anticoagulation, or antiplatelet drugs; Additional treatment/surgery from device-related complications; Bleeding; Blood disorders (including coagulopathy, hemolysis, and heparin induced thrombocytopenia (HIT)); Cardiac arrhythmias (including conduction disorders, atrial arrhythmias, ventricular arrhythmias); Cardiac ischemic conditions (including myocardial infarction, myocardial ischemia, unstable angina, and stable angina); Cardiac perforation; Cardiac tamponade; Chest pain; Death; Dyspnea; Edema; Embolization (device or components of the device); Endocarditis; Fever or hyperthermia; Fluoroscopy and transesophageal echocardiogram (TEE) related complications: Skin injury or tissue changes due to exposure to ionizing radiation, Esophageal irritation, Esophageal perforation, Gastrointestinal bleeding; Hypotension/hypertension; Infection including: Septicemia; Nausea or vomiting; Pain; Pericardial effusion; Stroke/cerebrovascular accident (CVA) and transient ischemic attack (TIA); System organ failure: Cardio-respiratory arrest, Worsening heart failure, Pulmonary congestion, Respiratory dysfunction or failure or atelectasis, Renal insufficiency or failure, Shock (including cardiogenic and anaphylactic); Thrombosis; Tricuspid valve complications, which may complicate or prevent later surgical repair, including: Chordal entanglement/rupture, Single leaflet device attachment (SLDA), Dislodgement of previously implanted devices, Tissue damage, Tricuspid valve stenosis, Worsening, persistent or residual regurgitation; Vascular access complications which may require additional intervention, including: Wound dehiscence, Bleeding of the access site, Arteriovenous fistula pseudoaneurysm, aneurysm, dissection, perforation (rupture), vascular occlusion, Embolism (air, thrombus), Peripheral nerve injury; Venous thrombosis (including deep vein thrombosis) and thromboembolism (including pulmonary embolism).