For select transplant-eligible patients, the HeartMate 3™ LVAD and heart transplant can serve as a complementary therapies, resulting in a net prolongation of life.1

Get the Real World Data
Net Prolongation of Life Starts with HeartMate 3 LVAD
A life-extending strategy for younger heart failure patients
HeartMate 3 LVAD shows two-year survival comparable to transplant in patients under 502 – giving younger heart failure patients more long-term support options.
What is Net Prolongation of Life?
Net prolongation of life refers to the strategy of implanting a Left Ventricular Assist Device (LVAD) in younger heart failure patients <50 with the goal of extending overall survival and potential for myocardial recovery by delaying a heart transplantation, either temporarily or long-term.
Based on clinical evidence, the strategy of leading with LVAD prior to heart transplantation should be considered for select younger heart failure patients.
Watch Video Now
The 2024 Intermacs Annual Report: What real-world data really says about survival with LVAD
In this video Dr. Manreet Kanwar and Dr. Francis Pagani discuss the role of HeartMate 3 LVAD therapy in a net prolongation of life strategy for patients under 50.
Why lead with a LVAD prior to heart transplantation to prolong life?
Transplant
Median survival for heart transplant patients is 12.4 years.3
Only 2.6% of patients receive a second heart transplant, and those who do experience worse outcomes.4
LVAD
Median survival for HeartMate 3 LVAD patients exceeds 5 years,5 with many living over 10+ years.*

For select patients under 50, a net prolongation of life strategy that delays heart transplantation is an ideal approach to extending meaningful life.
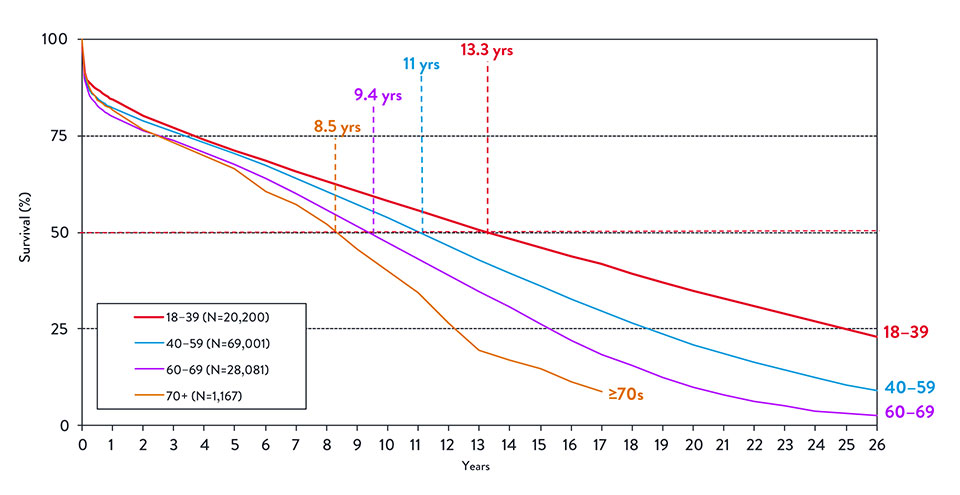
How long does a transplanted heart last?
Despite good survival outcomes for patients who receive a heart transplant, it may not be an ideal first option for younger patients.
Median survival for younger heart transplant patients is only 11-13 years. That means younger patients will likely need another transplant over their lifetime.3
Finally, the ability for patients to receive a secondary transplant is only 2.6% with the association of worse survival.4
How does HeartMate 3 LVAD make net prolongation of life possible?
The potential for offering a net prolongation of life strategy to select patients is made possible by high survival outcomes with the HeartMate 3 LVAD, especially in a younger patient population.
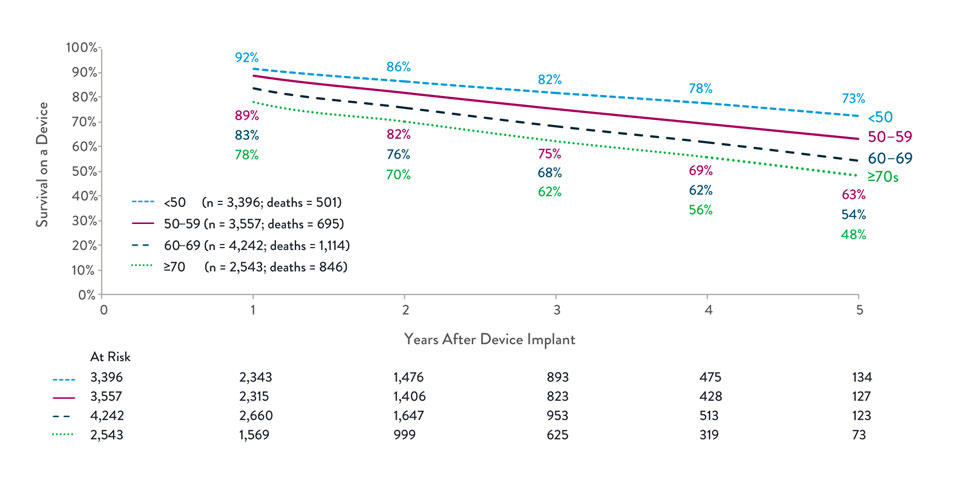
73%
survival at 5 years in patients <50 years old for HeartMate 3 LVAD1
See the real-world clinical evidence for HeartMate 3 LVAD
The Society of Thoracic Surgeons Intermacs 2024 Annual Report: Focus on Outcomes in Younger Patients

{hospital}
{distance} miles
Results
Clinics are listed in order of geographic proximity from the information entered in the locator. Abbott does not endorse any of the clinics on this locator, but merely provides them as a courtesy to patients. Nor does Abbott represent that this is a full list of clinics in a particular location. Though Abbott attempts to regularly update the locator, the locator may not have the latest information regarding the clinic or provider, or availability of product. The clinics are included in the locator because they are certified as a HeartMate LVAD implanting center, have ordered at least one HeartMate LVAD in the last 12 months, and have all HeartMate LVAD device-related equipment required for patient management. The number of orders has been validated; the number of implants has not been validated. This locator includes US clinics only. No clinics or healthcare professionals (HCPs) have paid or received a fee to be listed, but some HCPs within the clinics on this locator may purchase products from Abbott, provide consulting services to Abbott, and/or may have a financial relationship with Abbott. The locator is not meant to be an endorsement for any particular clinic, nor does it represent the qualifications of the HCPs at the clinic. Note that Abbott is a medical device manufacturer and cannot provide medical advice.
For more information about this clinic locator please see our policy. Any information you provide is covered by Abbott’s Privacy Policy
Intermacs is a North American longitudinal registry for the real-world clinical outcomes of patients who receive an FDA-approved mechanical circulatory support device to treat advanced heart failure. Registry does not include trial devices.
*Based on clinical trial and device tracking data as of August 8, 2025.
References
- Meyer DM , Nayak A, Wood KL, et al. The Society of Thoracic Surgeons Intermacs 2024 Annual Report: Focus on Outcomes in Younger Patients. Ann Thorac Surg. 2025;119(1):34-58.
- Uriel N. Survival outcomes in younger patients with advanced heart failure: a comparative analysis of HeartMate 3 LVAD and heart transplant using MOMENTUM 3 and UNOS registry data. Presented at: Annual Congress of the Heart Failure Association of the European Society of Cardiology; May 18, 2025; Belgrade, Serbia.
- Khush KK, Cherikh WS, Chambers DC, et al. The International Thoracic Organ Transplant Registry of the International Society for Heart and Lung Transplantation: Thirty-fifth Adult Heart Transplantation Report-2018; Focus Theme: Multiorgan Transplantation. J Heart Lung Transplant. 2018;37(10):1155-1168.
- Hess NR, Hickey GW, Sultan I, Kilic A. Redo orthotopic heart transplantation in the current era. J Thorac Cardiovasc Surg. 2023;166(2):583-594.e3. doi:10.1016/j.jtcvs.2021.09.061
- Mehra MR, Goldstein DJ, Cleveland JC, et al. Five-Year Outcomes in Patients With Fully Magnetically Levitated vs Axial-Flow Left Ventricular Assist Devices in the MOMENTUM 3 Randomized Trial. JAMA. September 8, 2022. doi:10.1001/jama.2022.16197)
- The International Society for Heart and Lung Transplantation. International Thoracic Organ Transplant (TTX) Registry Data Slides. ISHLT; 2018. Available from: https://www.ishlt.org/registries/international-thoracic-organ-transplant-%28ttx%29-registry
MAT-2511228 v1.0