Deployment & Suture Management
4 Key Steps to Suture Deployment
Refer to Instructions for Use (IFU) for additional information.

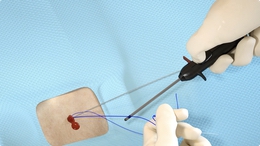
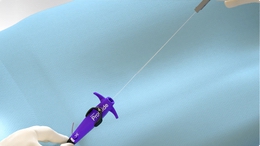
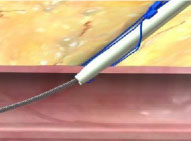
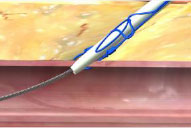
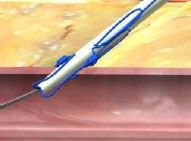
1. Advance device & lift Lever (Open Foot)
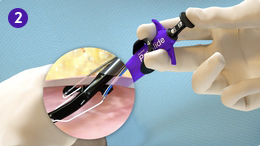
2. Maintain retraction and depress Plunger (Deploy Needles)

3. Pull back Plunger (Deploy Suture)

4. Lower Lever (Close Foot)
Suture Management
Refer to Instructions for Use (IFU) for additional information.
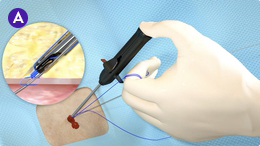
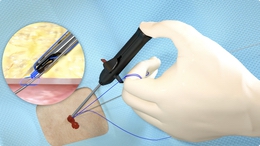
A. Capture blue (rail) suture limb in Suture Gate and advance Suture Knot
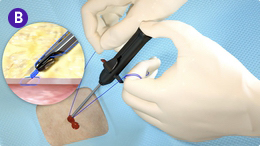
B. Lock Suture Knot by pulling white (non-rail) suture limb

C. Trim suture limbs by pulling Trimming Lever
Single and Multiple Device Deployment
Refer to Instructions for Use (IFU) for additional information.
View the animation library for full deployment steps for single and multiple devices.
Single Device Deployment
Multiple Device Deployment
Tips and Techniques
Refer to Instructions for Use for additional information.
Poor Flow
Arterial Poor Flow

Causes
- Marker Port is against the vessel wall
- Side wall stick
- Low blood pressure
- Clot or tissue plugging Marker Port
- Device not in vessel lumen
Venous Poor Flow

Resolution For Poor Flow
- If vessel is not ≥ 5 mm, do not deploy
- Gently rotate device
- Slow drip is acceptable
- Retract device until Marker Port is above skin. Re-flush Marker Lumen and observe saline exit Marker Port
- Continue inserting device until brisk pulsatile flow occurs in the artery and slow drip occurs in the vein
Suture Break
Causes/Prevention

- Suture may look thin and elongated
- Rail or non-rail limbs can break
- Load Suture at mid-point of Suture Trimmer (Do not load at tip)
- Keep Thumb Knob retracted until Suture limbs drop into Suture Gate (Do not close Suture Gate on the Suture)
- Keep Thumb Knob toward ceiling (Do not rotate Suture Trimmer)
- Keep suture limbs coaxial to Suture Trimmer and tissue tract at all times
- Do not pull laterally or medially on Suture
- Apply slow, consistent, increasing tension (Avoid quick, jerky movements)
Resolution

- If the device is still in place
Insert wire and exchange for another device - If closing over the wire
Insert and deploy another device - If device is already removed and no wire access, assess hemostasis
Manual compression may be necessary, depending on when and where the Suture broke
Cuff Miss
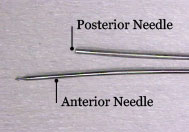
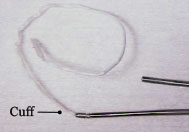
- Plunger is withdrawn and no Suture is present. The link may or may not be attached to Anterior Needle
- Tip(s) of Needle(s) did not lock with Cuff(s)
Prevention

- Proper patient selection
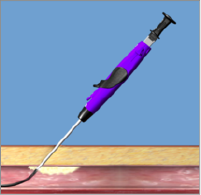
- Deploy device at 45° stabilize device with left hand during Plunger deployment

- Ensure black Collar on Plunger contacts purple Body
- Maintain and stabilize the device at 45° throughout removal of Plunger/Needles and until Suture is fully retracted
Resolution
- Insert wire and exchange for another device
Foot Break
Causes/Observations
Potential causes during Plunger deployment (Step 2)
- Rotating/rocking the device or excessive force during Plunger deployment
- Shallow (less than 45º) Plunger deployment angle


Potential observations after Plunger removal (Step 3) and/or device removal
- No Suture or link present
- Just a link and no Suture present
- Missing part of Foot when the device is removed
Prevention

- Stable and position the device at 45º angle during Plunger deployment
- The deployment angle may vary slightly depending on anatomy
- Maintain even and gentle tension over the Anterior and Posterior Foot against the vessel wall
- The key is to raise the device until pressure is evenly distributed across the Anterior and Posterior Foot
- Press down on the Plunger with a gentle, increasing pressure to advance the Needles
- The Needles are more susceptible to deflecting off calcification with higher Plunger force and higher Needle speed
Deployment Angle During plunger deployment (Step 2)
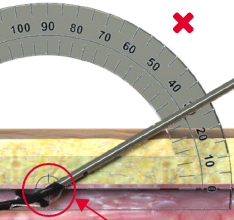
 Shallow Deployment Angle
Shallow Deployment Angle
- Sub-optimal in any tissue conditions
- Potential gap between Posterior Foot and vessel wall increases chance for foot break and cuff miss
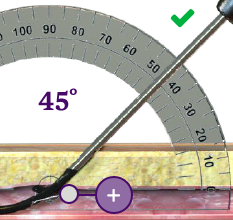
 45º Deployment Angle
45º Deployment Angle
- Ideal in healthy compliant tissue conditions
- Posterior and Anterior Foot appose evenly to compliant vessel wall
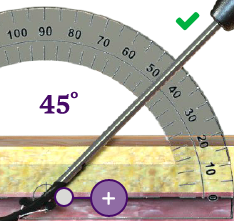
- Important in diseased non-compliant tissue conditions
- Maintain even and gentle tension to position Posterior Foot close to non-compliant vessel wall
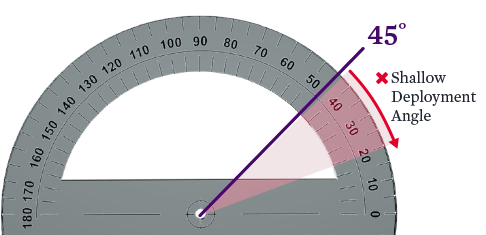
Exercise:
Use an actual device, observe the different foot deployment angles
Note: Best if protractor is viewed on a small screen or print out
Foot Break Prevention
- Avoid challenging anatomical conditions such as heavily calcified arteries, scarred groins, etc
- These conditions may make the Needles more susceptible to deflecting

Before attempting to remove the device:
- Relax the device before pushing the Lever down
- Push the Lever down to return Foot to the closed position

Lack of Hemostasis
Lack of hemostasis may be a result of incorrect order of knot advancement or tangled sutures.
Incorrect Order of Knot Advancement
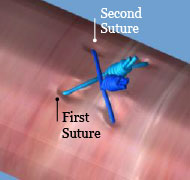
- Advance Sutures in the order of deployment
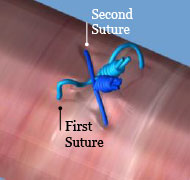
- First Suture deployed is on the "bottom" or closest to the vessel. If Second Suture is tightened out of order, it may result in tangled Sutures and/or the inability to tighten the First Suture successfully
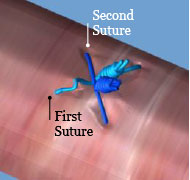
- After initial knot advancement of all Sutures, continue to tighten and lock each knot in the order deployed
- Tightening and locking the Second Suture before the First Suture is completely secure can result in an incomplete or "partial" close
Tangled Sutures
- After Suture Deployment, a clamp is immediately placed on the Suture limbs. A gentle retraction is placed on the clamp until the Suture is taut. This removes all Suture slack from the tissue tract
- If Suture slack is not removed, the Sutures can become tangled or pushed into the vessel during insertion of procedural sheaths and device exchanges
References
- Perclose ProGlide - Instructions for Use (IFU). Refer to IFU for additional information.
MAT-2103419 v3.0