Case Images
These case images show some of the imaging possibilities of the Advisor™ HD Grid Mapping Catheter, Sensor Enabled™:
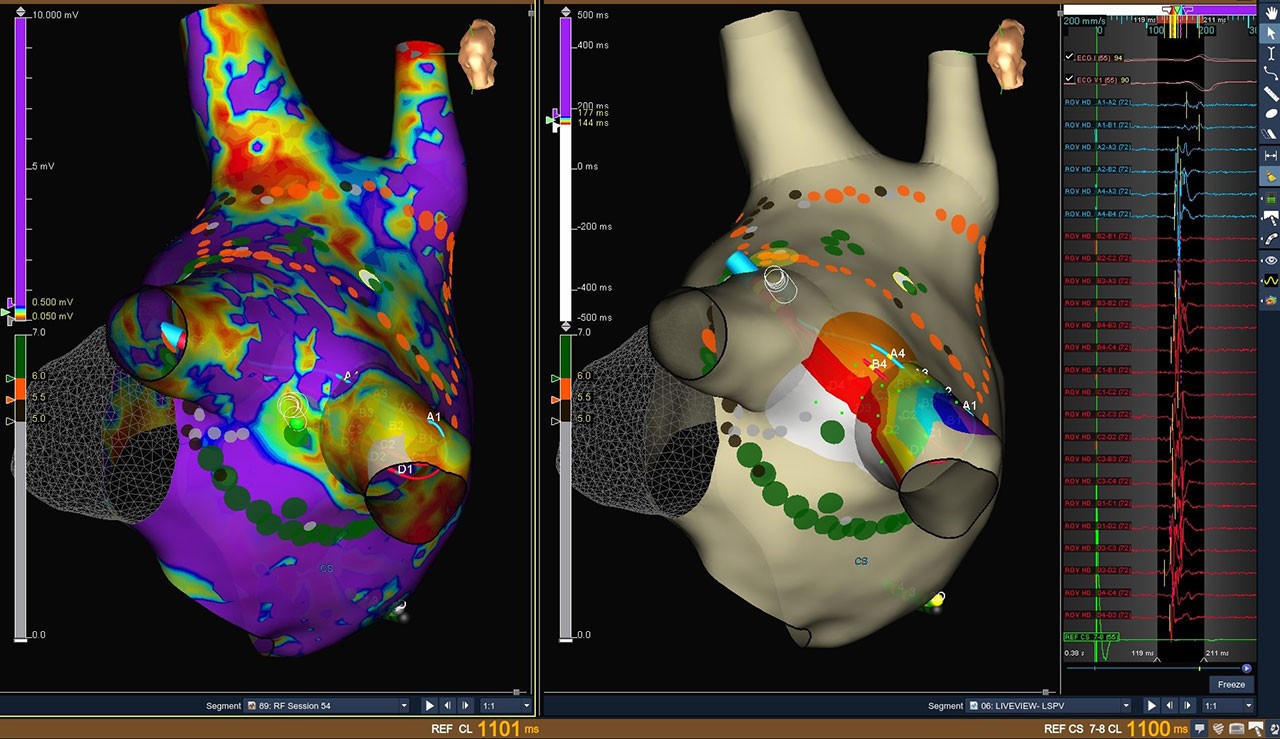
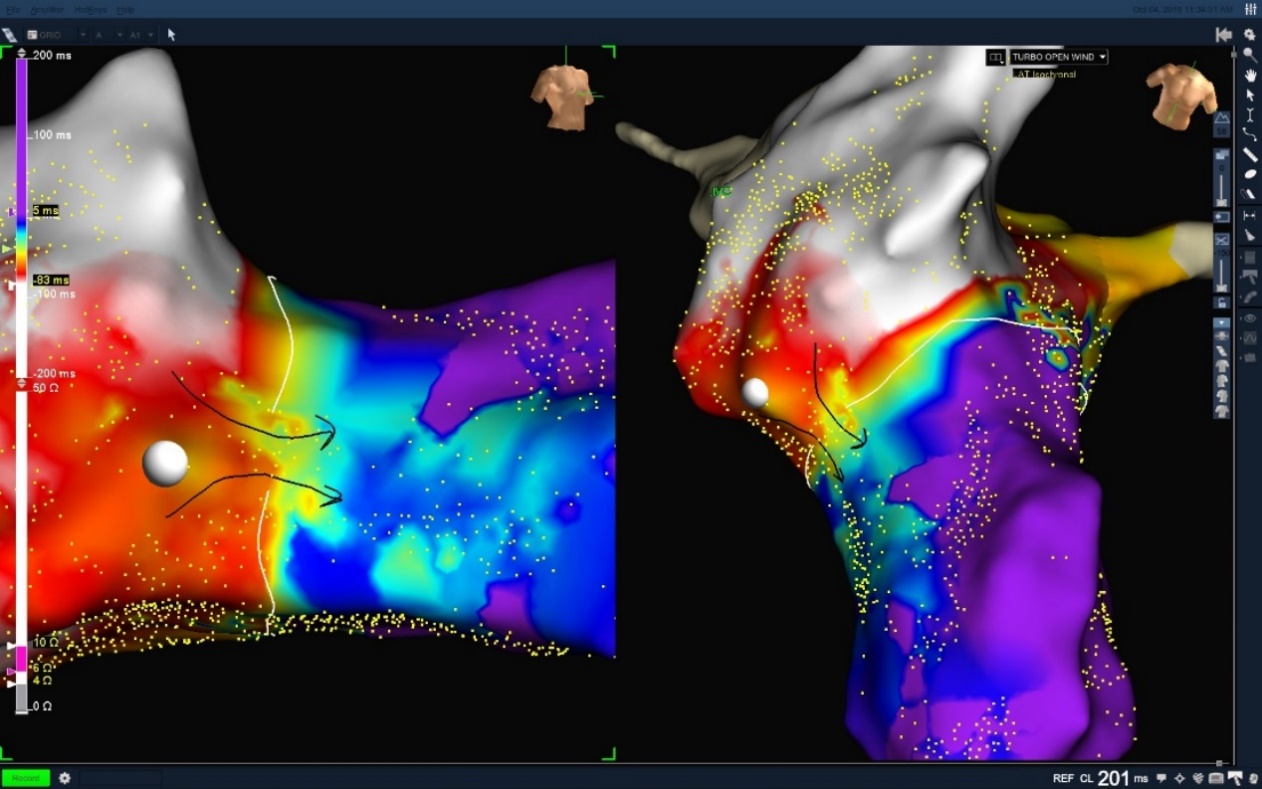
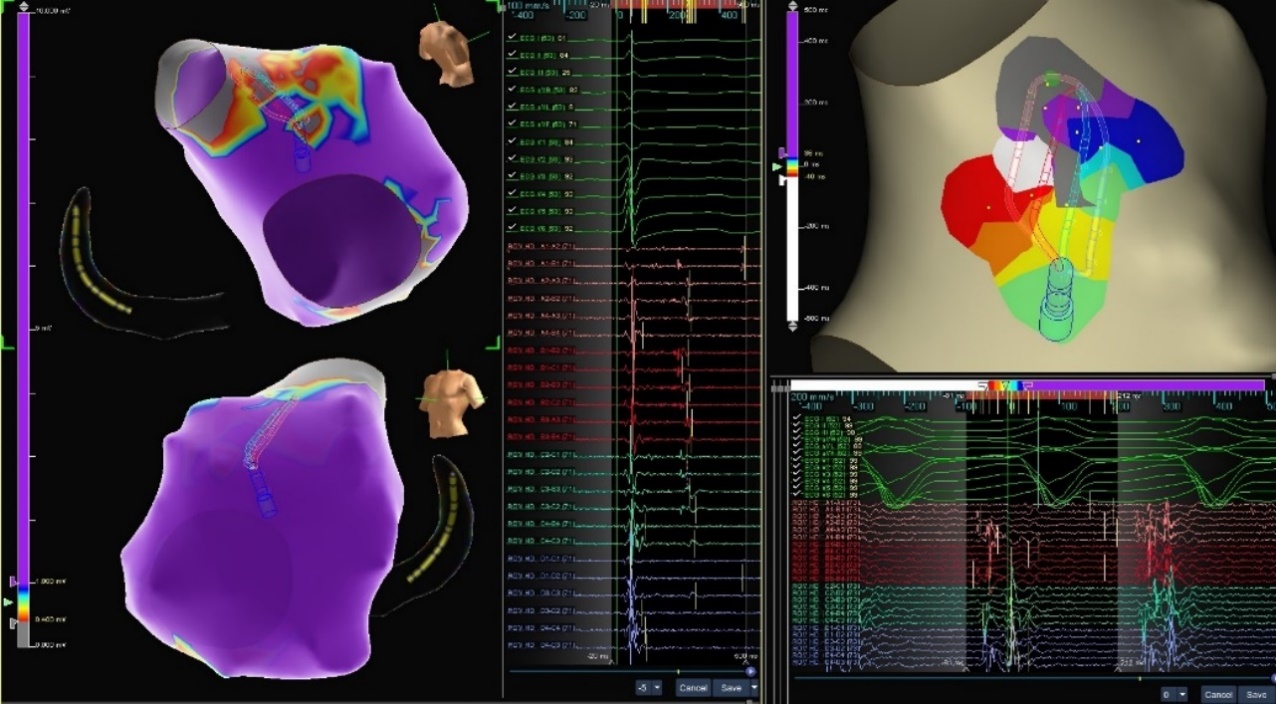
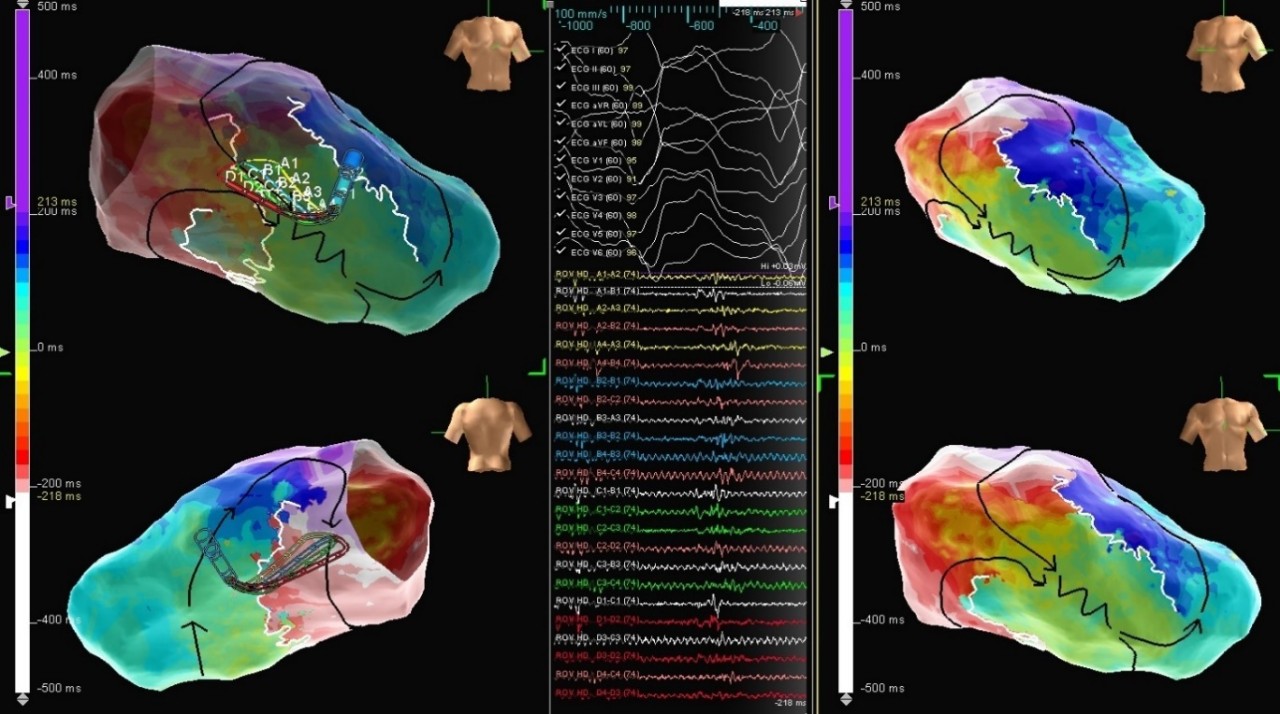
LiveView Dynamic Display

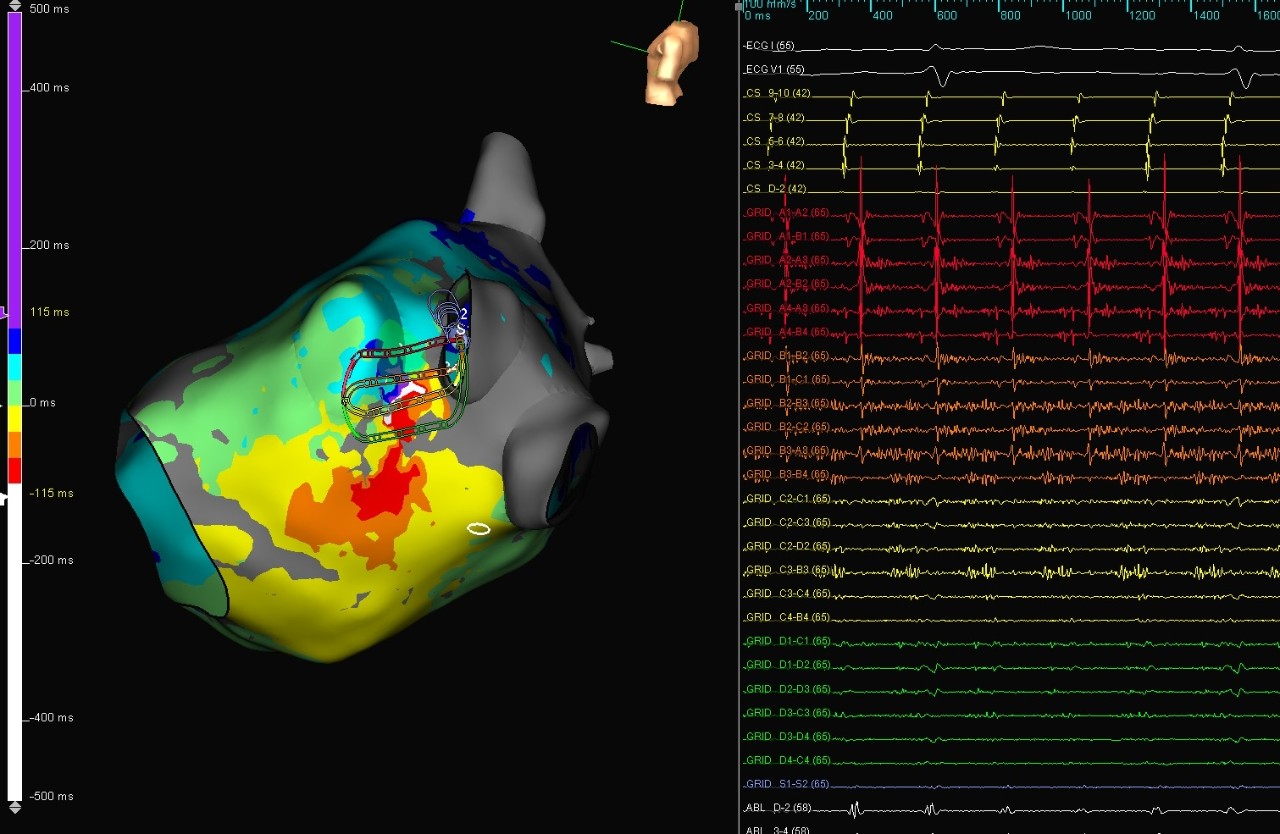
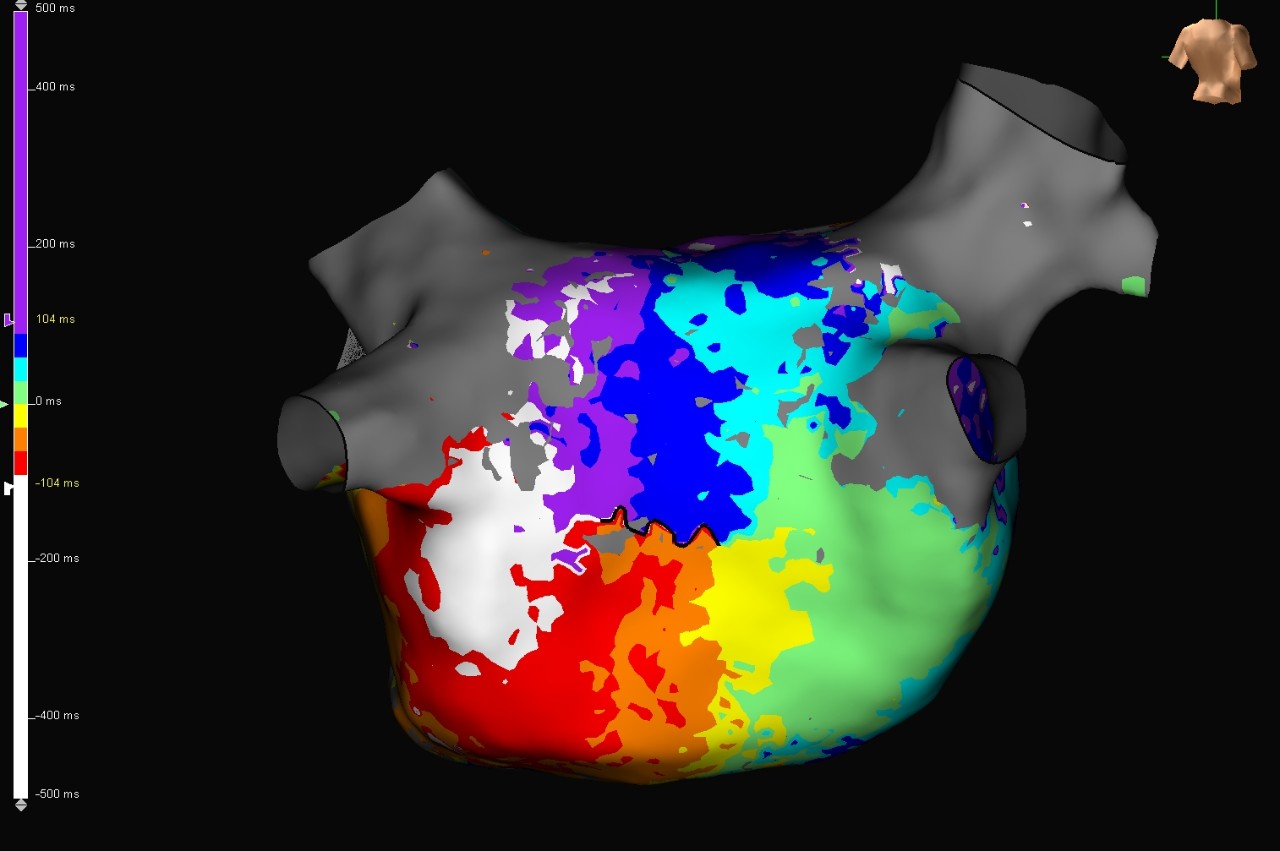
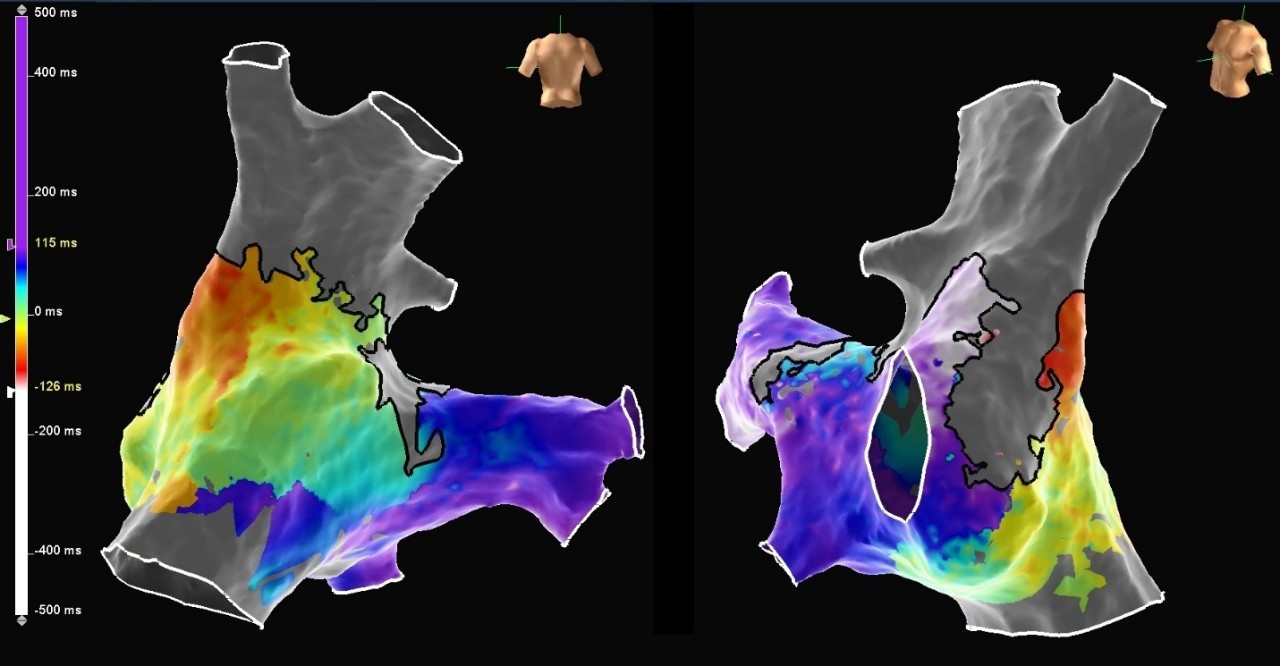
Atrial Fibrillation
LiveView Dynamic Display + Advisor HD Grid Mapping Catheter, SE were used in this case for a patient with persistent atrial fibrillation. WACA ablation was performed and a posterior wall isolation was added following the discovery of fractionated EGMs during the case. With Advisor HD Grid Mapping Catheter, SE sitting in the pulmonary vein during ablation, LiveView Dynamic Display helped the physician visualize functional changes in how the wavefront was propagating into the vein, helping to confirm lines of block as they were created. LiveView Dynamic Display also helped to highlight areas to focus on during ablation in order to achieve isolation in real time without additional mapping. During the posterior wall isolation, LiveView helped to quickly locate the source of an epicardial connection and achieve isolation causing for an audible cheer from the physician!
Image courtesy of Dr. Andres Enriquez (Kingston Health Sciences Centre | Ontario, Canada)
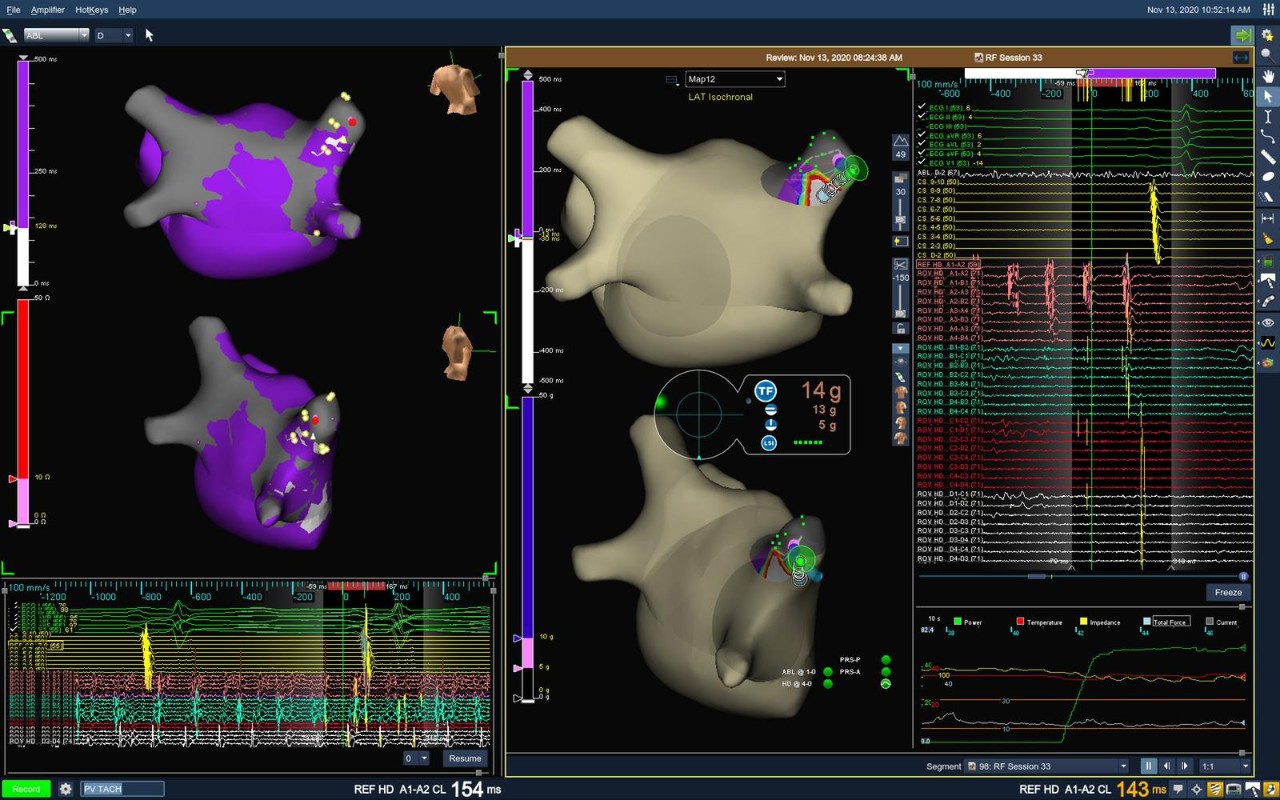
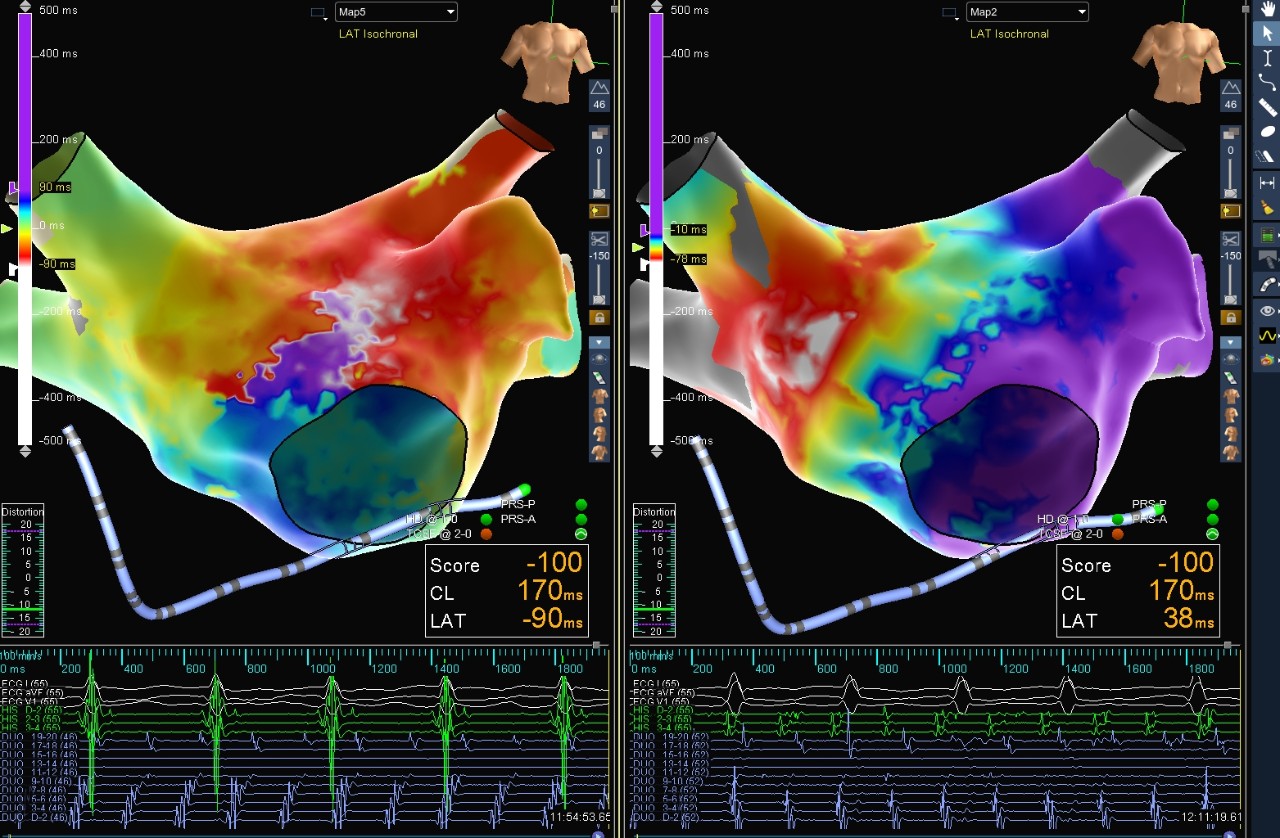
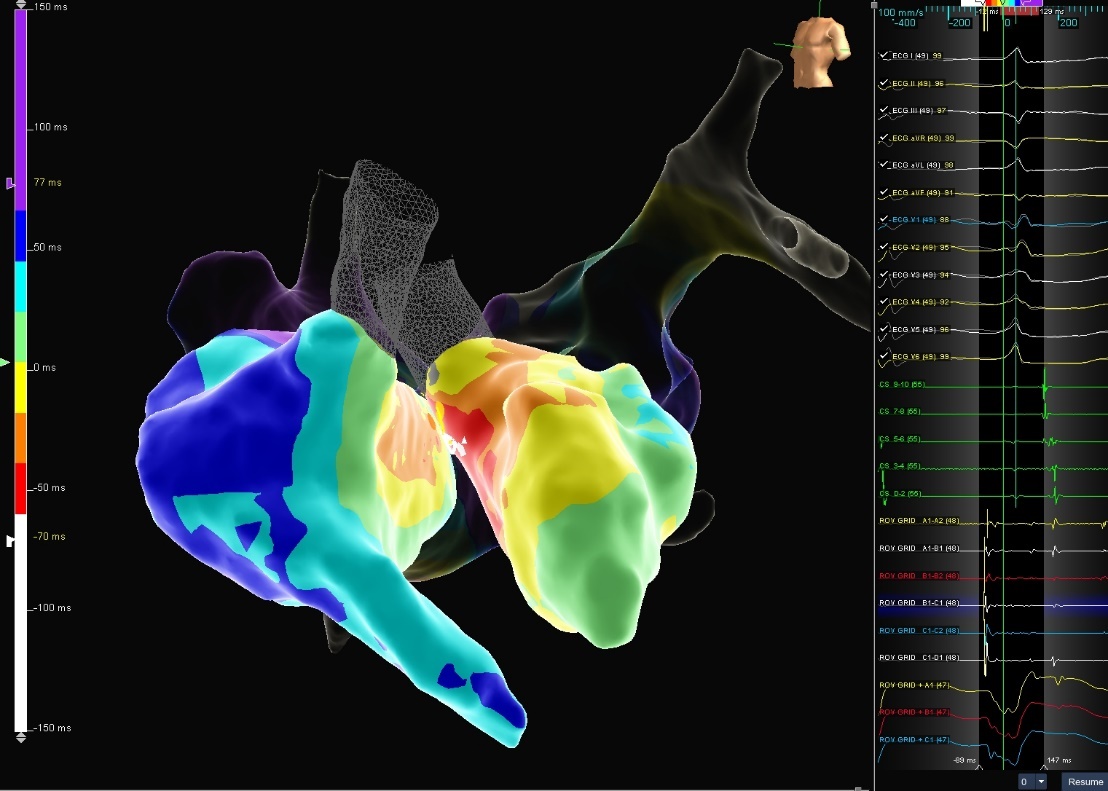
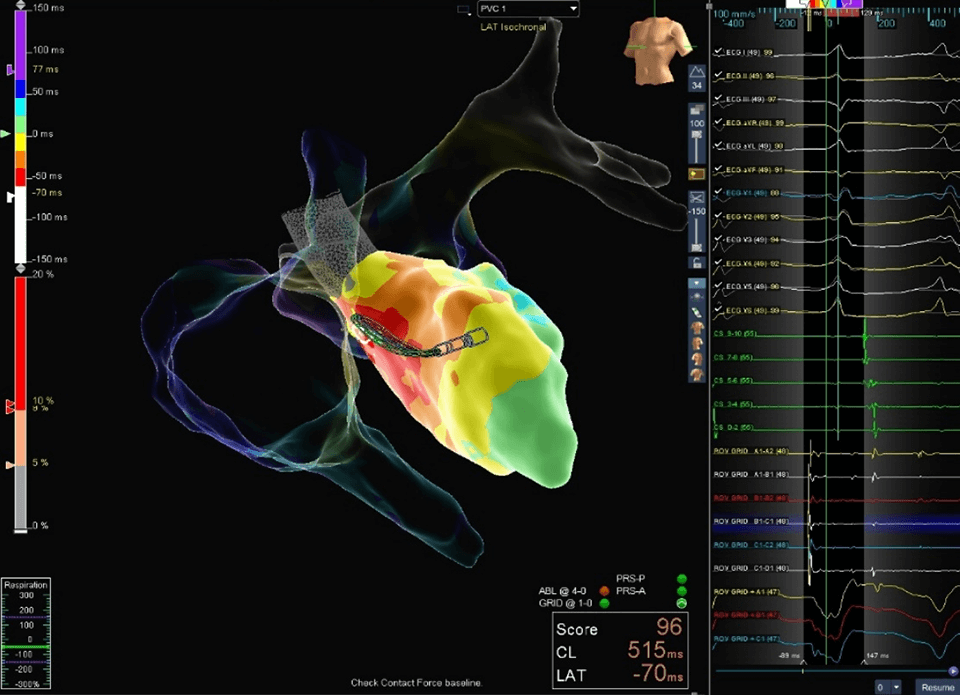
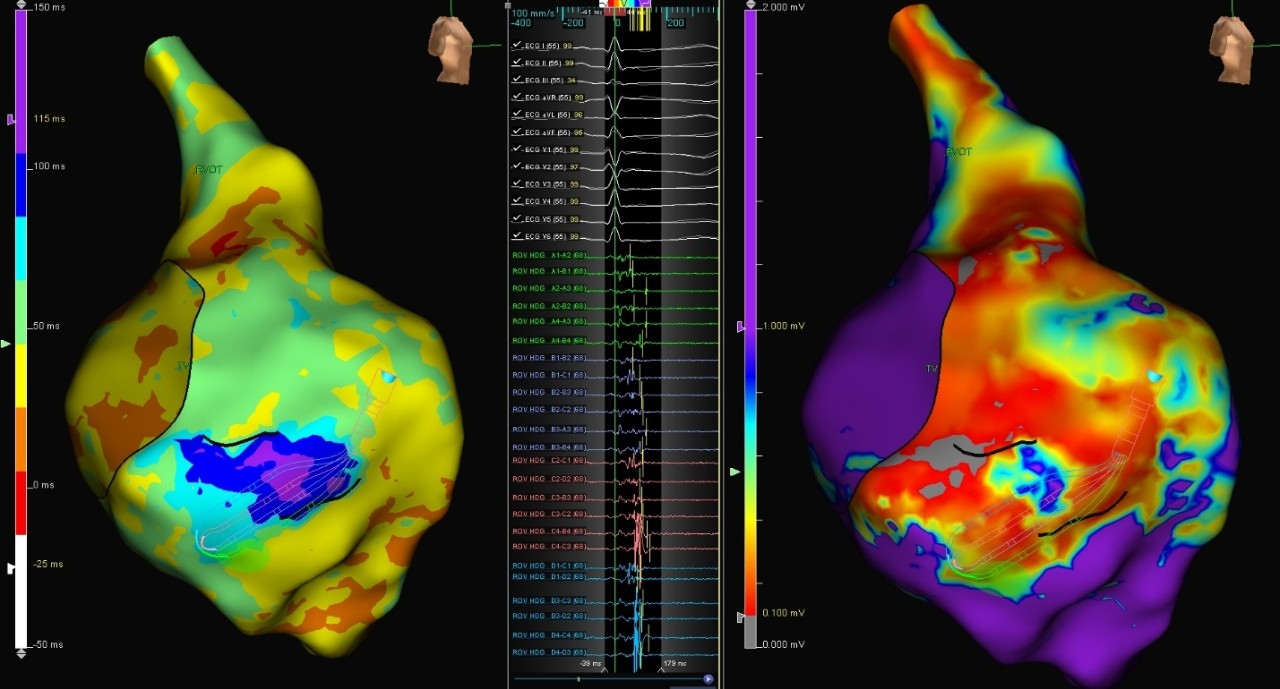
Paroxysmal AFib
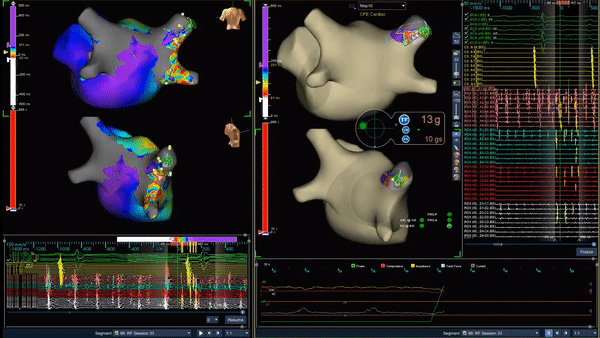
Paroxysmal AFib
This patient presented to the EP lab for a planned pulmonary vein isolation (PVI) procedure with roof line due to episodes of symptomatic paroxysmal atrial fibrillation. An initial map and model of the left atrium was created using the Advisor HD Grid Mapping Catheter, SE. PVI and roof line were completed using the TactiCath Contact Force Ablation Catheter, SE and the AutoMark Module to help target a force measurement between 10 and 30 grams and an impedance drop of greater than 10 ohms. This video shows continuation of AFib in the right superior pulmonary vein (RSPV) following successful PVI. Synchronized cardioversion of the vein was attempted at 100 J with temporary success, but AFib reinitiated within the isolated RSPV following a 12 mg bolus of adensoine. At that point, HD Grid and the LiveView Dynamic Display software were used to target the site of earliest activation and consistent fractionation within the vein. Ablation at the LiveView-suggested target site led to the termination of vein AFib within 3 seconds.
Image courtesy of Dr. Ashit Patel (Cascade Cardiology | Salem, OR)
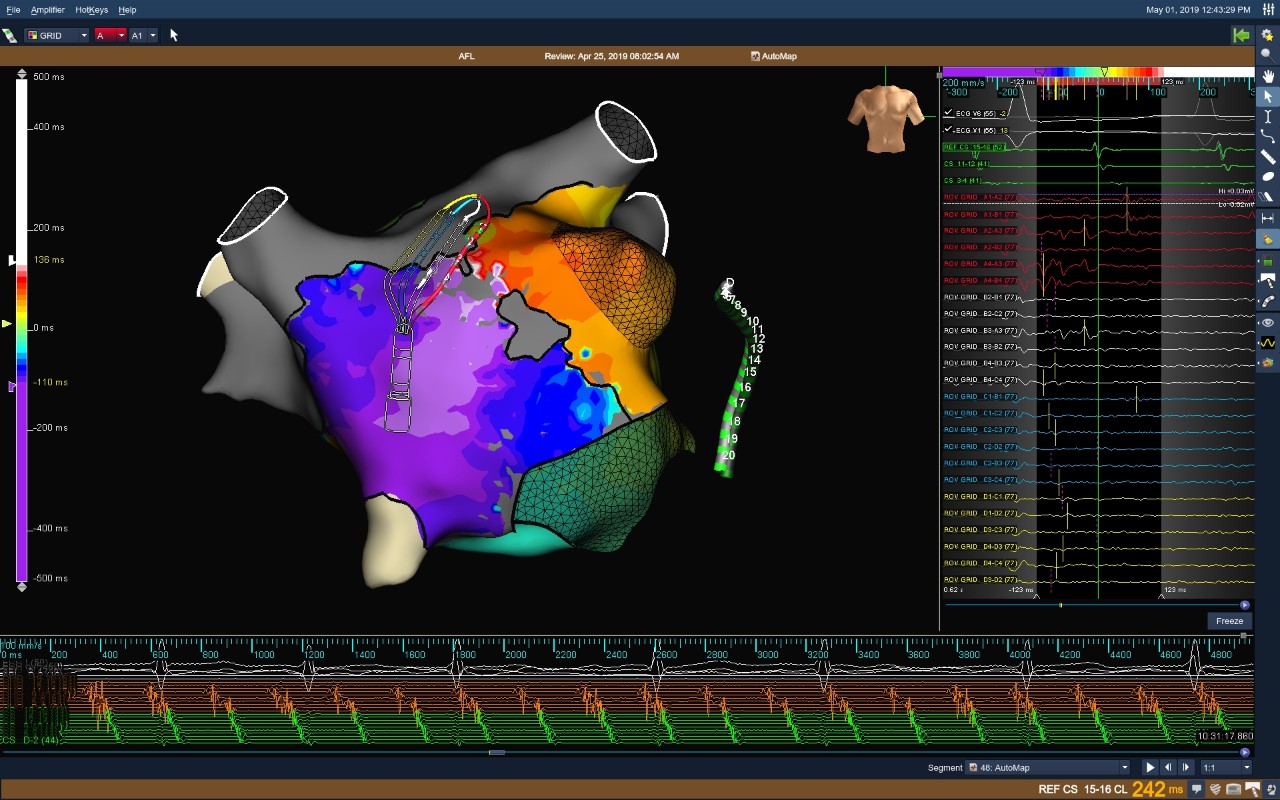
AFL Left Atrium Map
Atypical AFL
This patient presented to the EP lab following bio-prosthetic mitral valve replacement and prior Maze procedure. A high-density map of the LA was completed using the Advisor HD Grid Mapping Catheter, SE. This map helped to identify a critical area of slow conduction directly adjacent to the inferior portion of the mitral valve annulus. Additionally, the HD Grid helped distinguish the many areas of dense scar and complex lines of block consistent with this patient’s history. A single ablation lesion in the area of slow conduction terminated this rhythm.
Image courtesy of Dr. Lim Toon Wei (National University Hospital | Singapore)
Full Contact Diagram
Atypical AFL
This patient presented to the EP lab in an atrial flutter subsequent to a prior mitral valve replacement and Maze procedure. A high-density map of the left atrium created using the Advisor HD Grid Mapping Catheter, SE, showed that the dominant circuit was counterclockwise mitral annular flutter. The high-density map also revealed gaps in the existing lesion set of the left-sided veins, with a wavefront entering at the inferior portion of the LIPV, exiting at the superior and anterior portion of the LSPV, and then colliding with the wavefront traveling around the mitral valve annulus. EGMs recorded near the gap in the LIPV highlight the importance of directionality during the recording of bipolar EGMs, as the EGMs between splines were up to three times larger in amplitude than the related down-spline EGMs. The flutter was terminated with a lesion set along the lateral mitral isthmus, anchored by a lesion in the gap in the LIPV.
Image courtesy of Dr. Eric Lim (National Heart Center | Singapore)
Double Loop in the Left Atrium
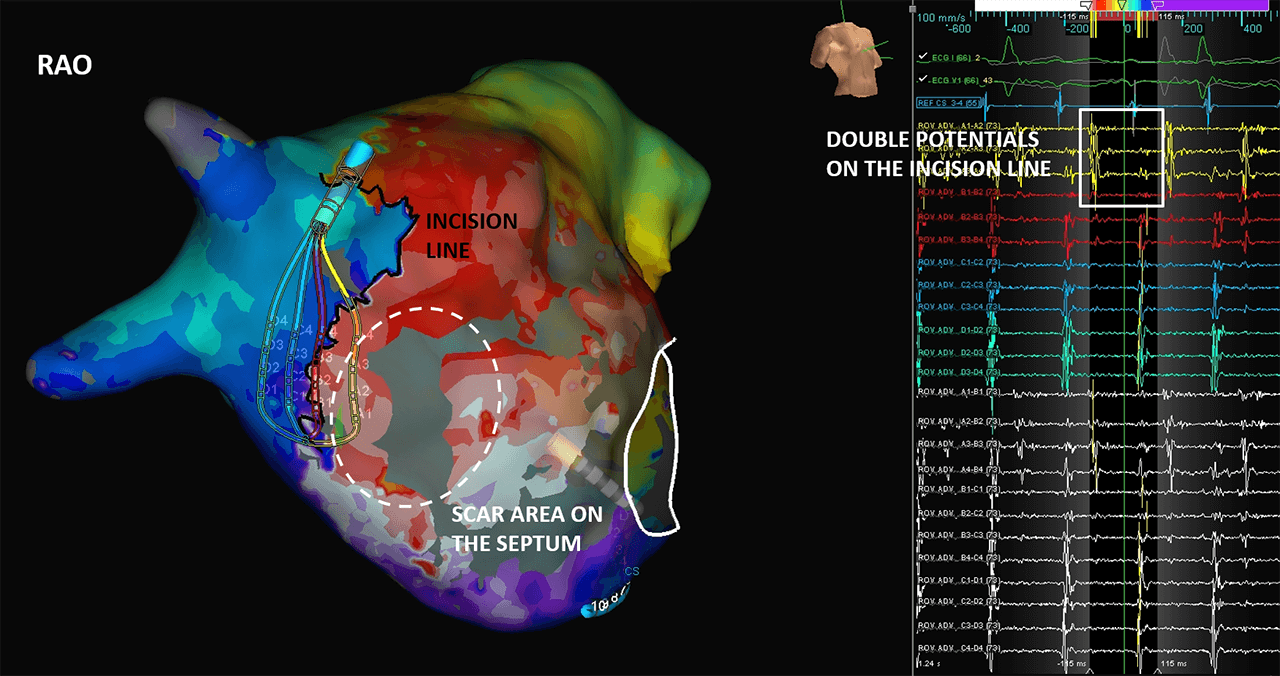
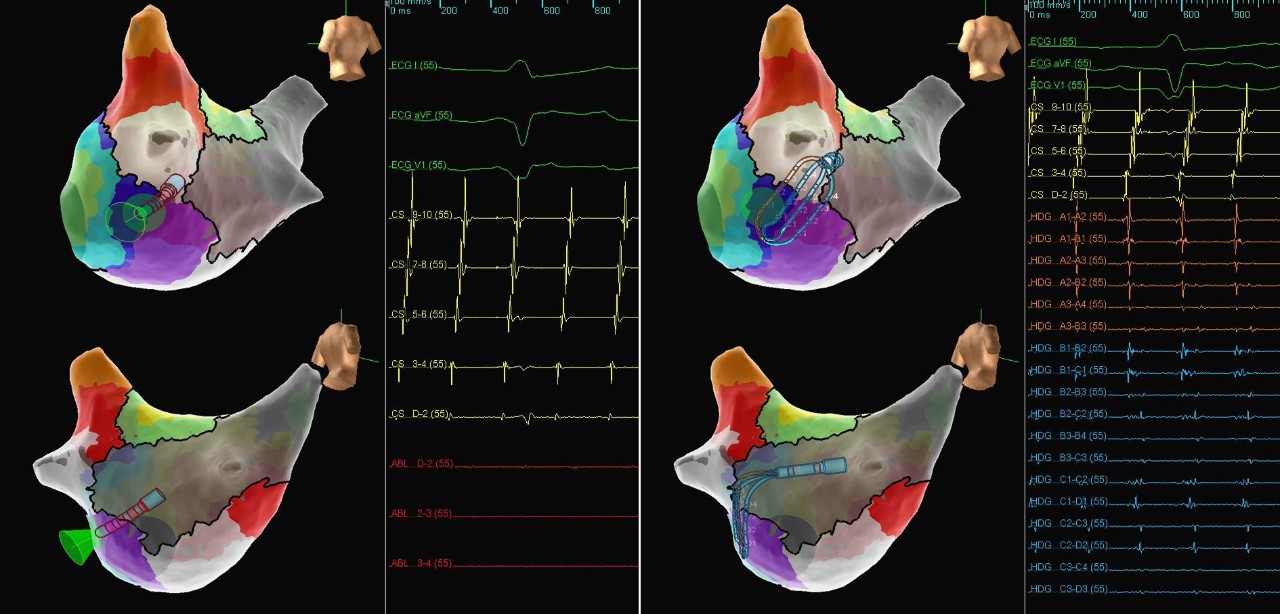
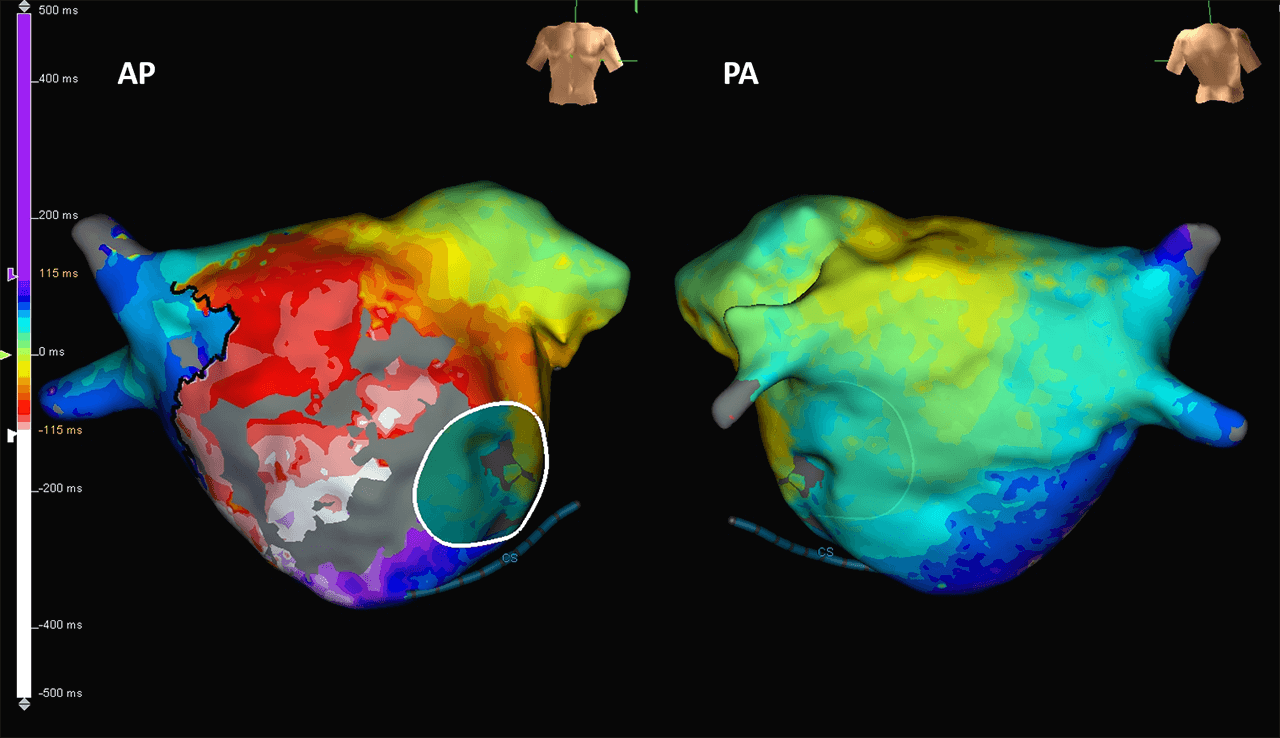
Atypical Atrial Flutter after ASD Repair
This case shows a patient with a mitral valve repair and an atrioventricular septal defect correction who presented in flutter. Using the Advisor HD Grid, Sensor Enabled, LAT maps were created to reveal a double loop around the mitral valve and the septal incision, a reentry on the CTI and on the RA septum passing through the lateral incision. Sinus rhythm was restored at the end of the procedure.
Image courtesy of Dr. J. Bertrand and Dr. M. Becker (CHR Mercy | Metz, FR)
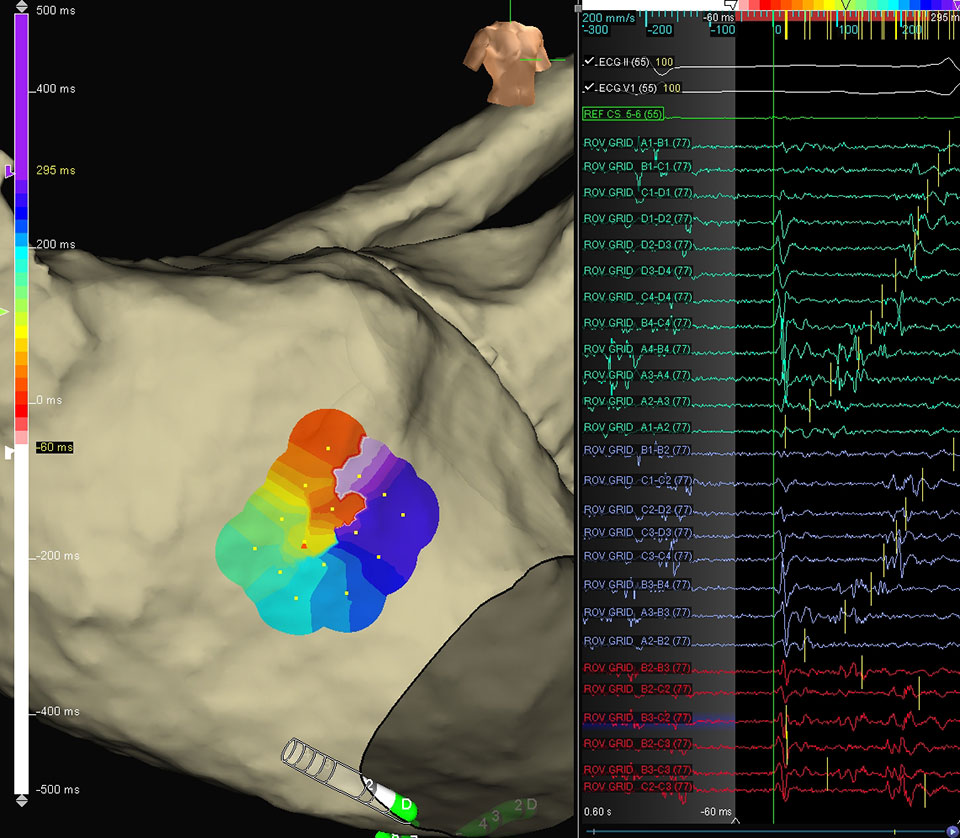
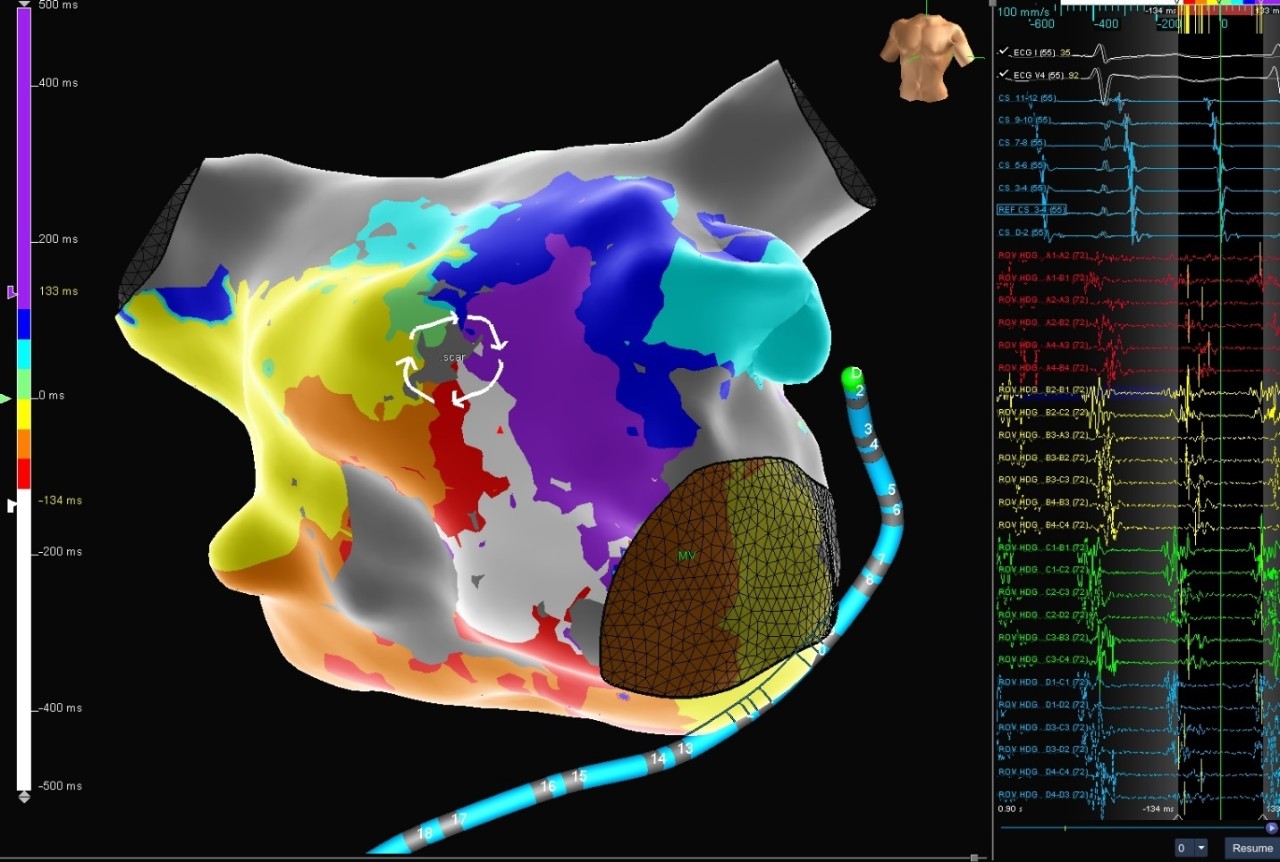
Left Atrial Micro-reentrant Flutter
Left Atrial Microreentrant Flutter
The patient was presented in Left Atrial Micro-reentrant flutter. Below shows a visual configuration of rotational activation, as demonstrated by the Advisor HD Grid Mapping Catheter, Sensor Enabled. When this micro-reentrant rhythm was induced, both continuous activation along the central bipoles (red electrograms) as well as clear movement around the outer edges of the Advisor HD Grid Mapping Catheter, Sensor Enabled (turquoise and purple electrograms) were visualized. The physician noted how helpful it was to get a full patch of information, showing both the inner slow conduction and the outer propagation.
Image courtesy of Dr. Stavros Mountantonakis (Lenox Hill Hospital | New York, NY)
LAT Maps of the LA
Atypical AFL
This patient, presented in atypical atrial flutter, had two prior Left Atrium (LA) ablations a decade ago and was arrhythmia free until recently. The Advisor HD Grid Mapping Catheter, Sensor Enabled was used to create multiple reentrant LAT maps of the LA, thus making the case by being able to quickly and accurately identify the region of scar and the flutter activation patterns. The image shows one of the circuits pinwheeling around scar tissue on the anterior wall. The tachycardia was terminated with the first RF ablation lesion.
Image courtesy of Dr. Sean Beinart (Adventist HealthCare White Oak Medical Center | Silver Spring, MD)
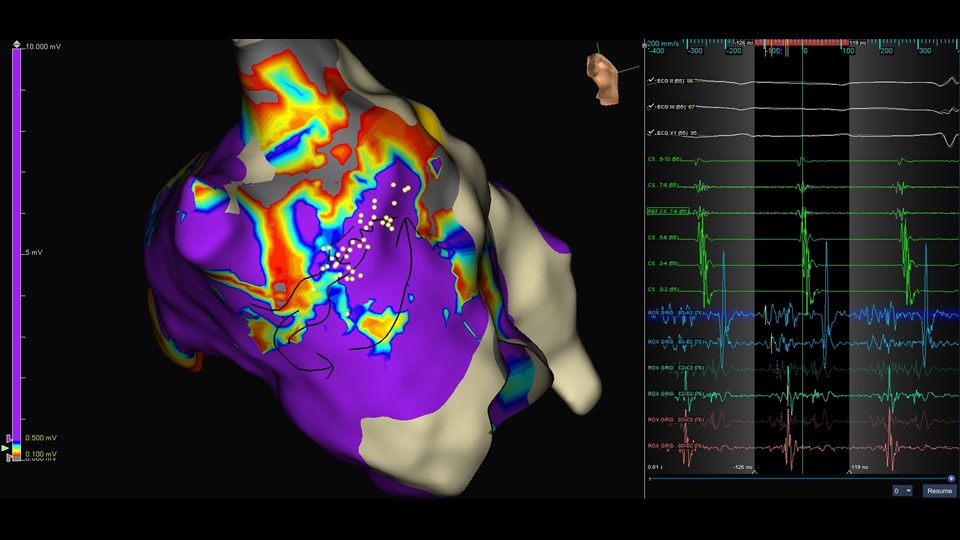
LAT Map
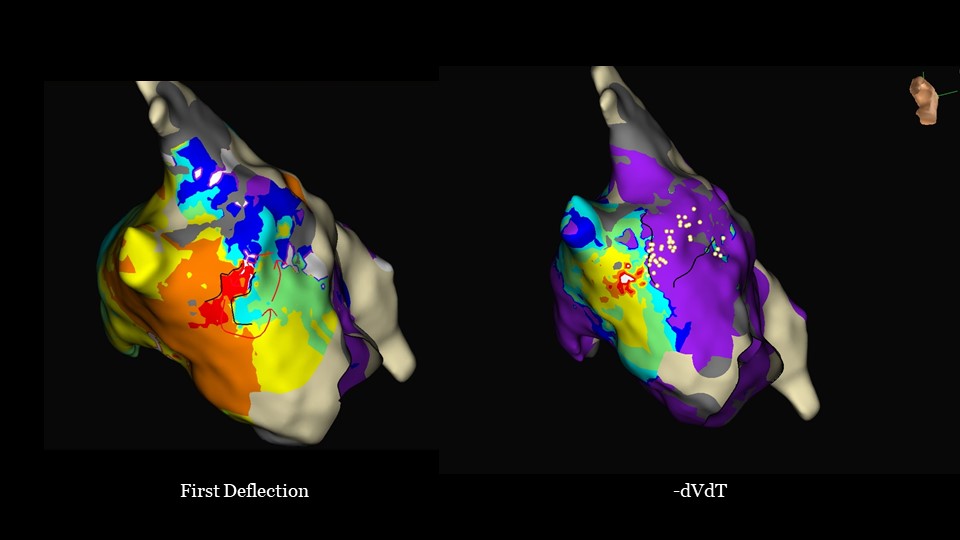
LA Septal Micro Re-entry
This patient underwent redo pulmonary vein isolation. During substrate mapping of the left atrium with the Advisor HD Grid Mapping Catheter, Sensor Enabled, an organized tachycardia was induced. An LAT map was initially produced using the ‑dVdT detection algorithm. This clearly identified an area of fractionated signal spanning 80% cycle length. Then TurboMap was used to reanalyze the map via the First Deflection algorithm, clearly identifying a channel along the septum, anterior to the RLPV.
Image courtesy of Dr. Stephen Page (Leeds Teaching Hospitals | Leeds, UK)
LAA Reentry
This patient, with a history of a prior maze procedure and a LAA ligation, was presented in left-sided atypical flutter. Long fractionated and nearly continuous electrograms were visible with the Advisor HD Grid Mapping Catheter, Sensor Enabled catheter near the ridge and the LAA stump. Immediate termination was achieved with RF ablation.
Image courtesy of Dr. Benzy Padanilam (Ascension St. Vincent Hospital | Indianapolis, IN)
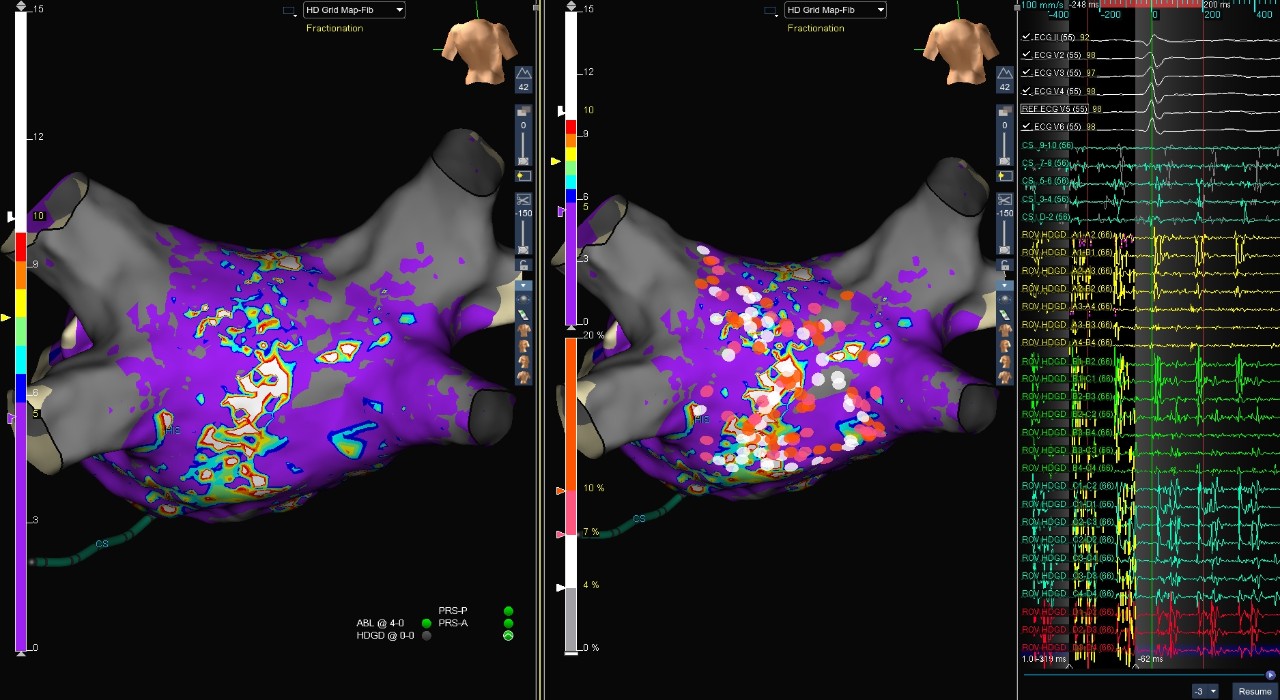
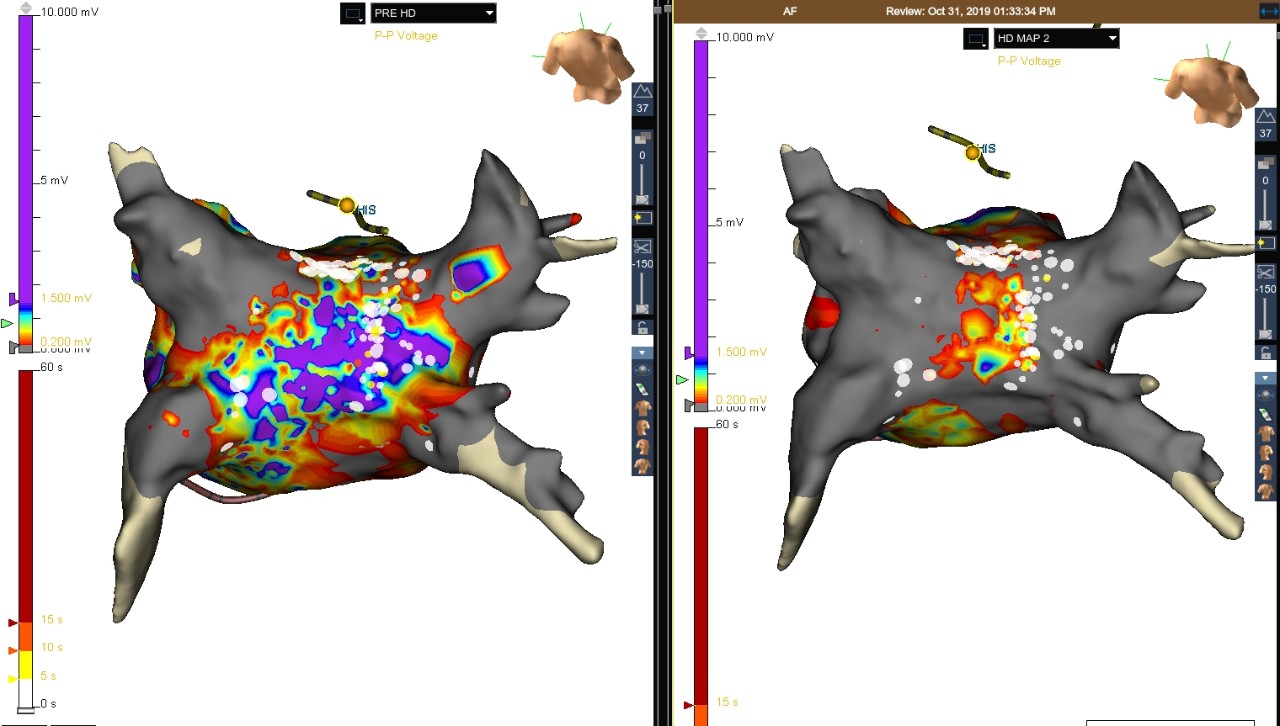
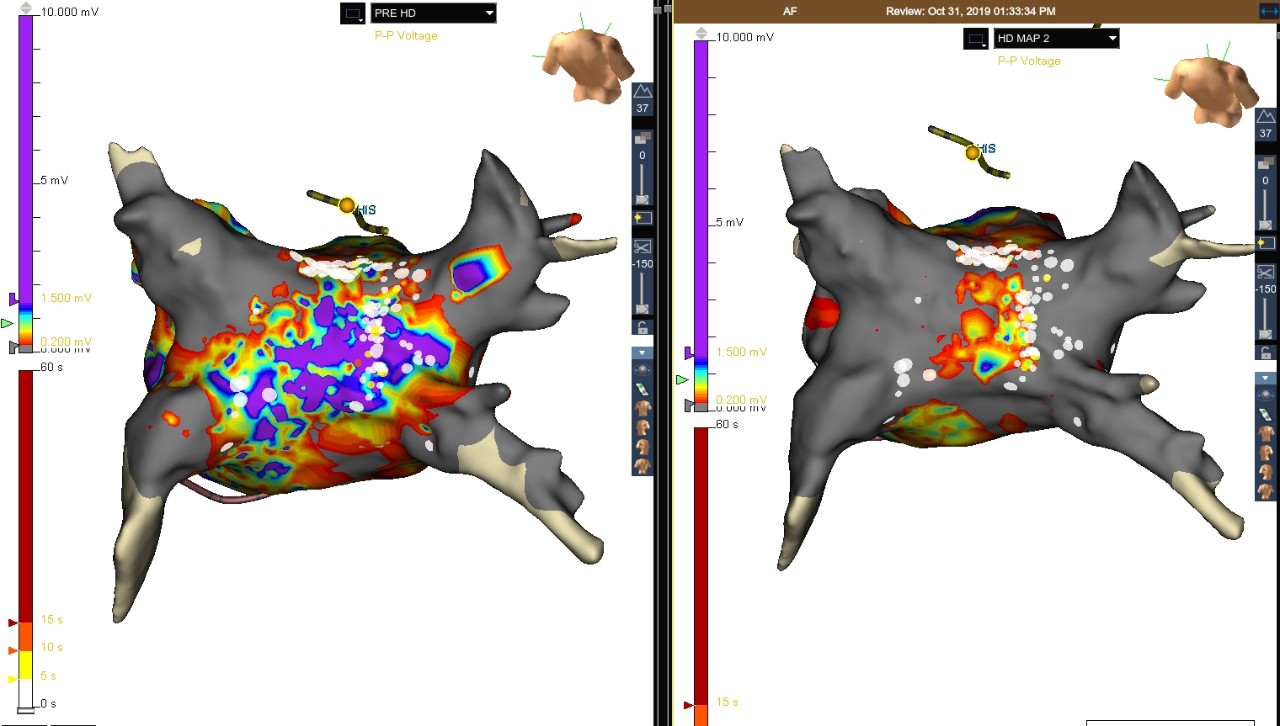
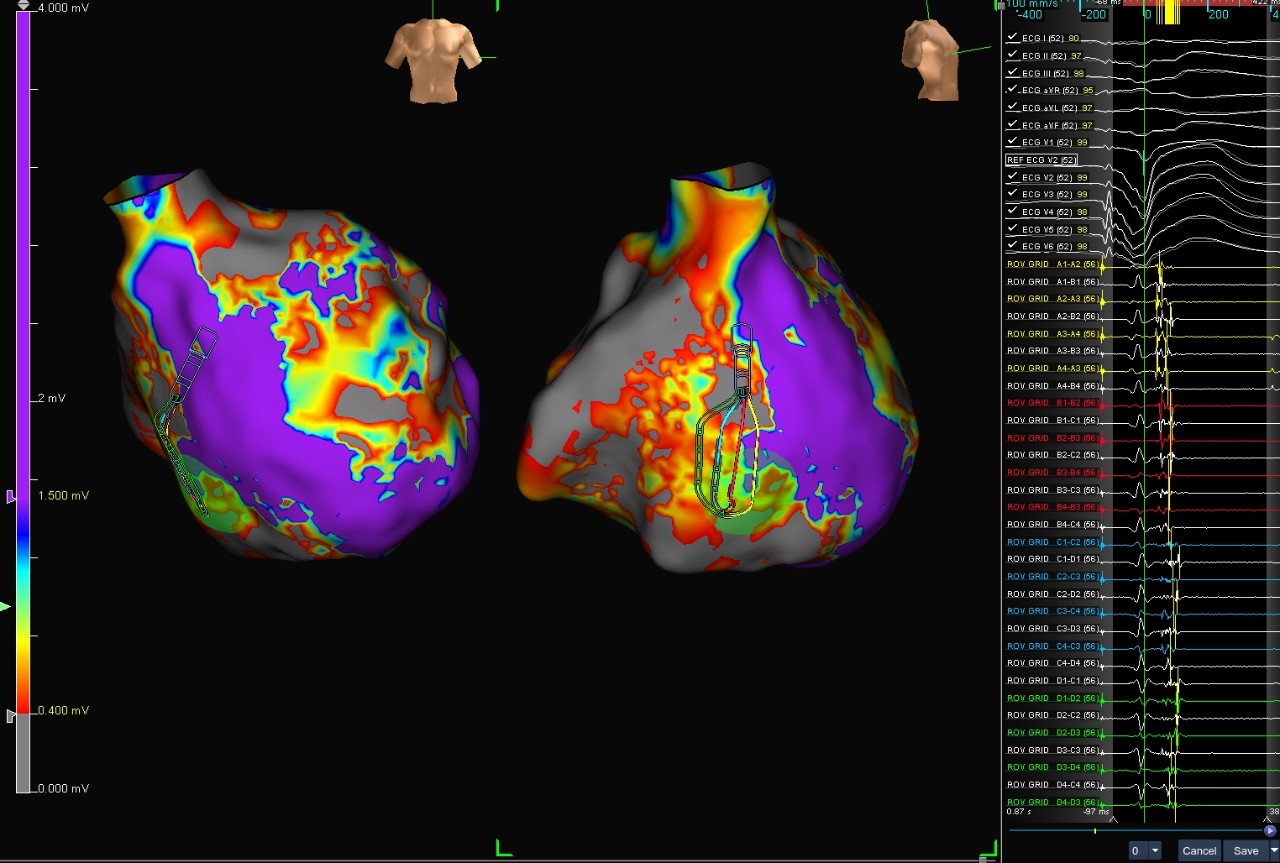
Voltage and Fractionation Map
Atrial Fibrillation
This case shows a patient who presented in AFib for a cryoballoon PVI. After cardioversions failed to restore normal sinus rhythm (NSR) post-ablation, physicians used the Advisor HD Grid Mapping Catheter, SE to create a voltage and fractionation map.
Geometry collected with the Advisor HD Grid Mapping Catheter, SE revealed the cryoballoon ablation missed the RIPV. What appeared to be the RIPV during the cryoballoon ablation was actually a middle branch. Substrate modification of highly fractionated zones was performed with RF ablation and NSR was restored.
Image courtesy of Dr. Thomas Crawford (University of Michigan Hospital and Health Center | Ann Arbor, MI)
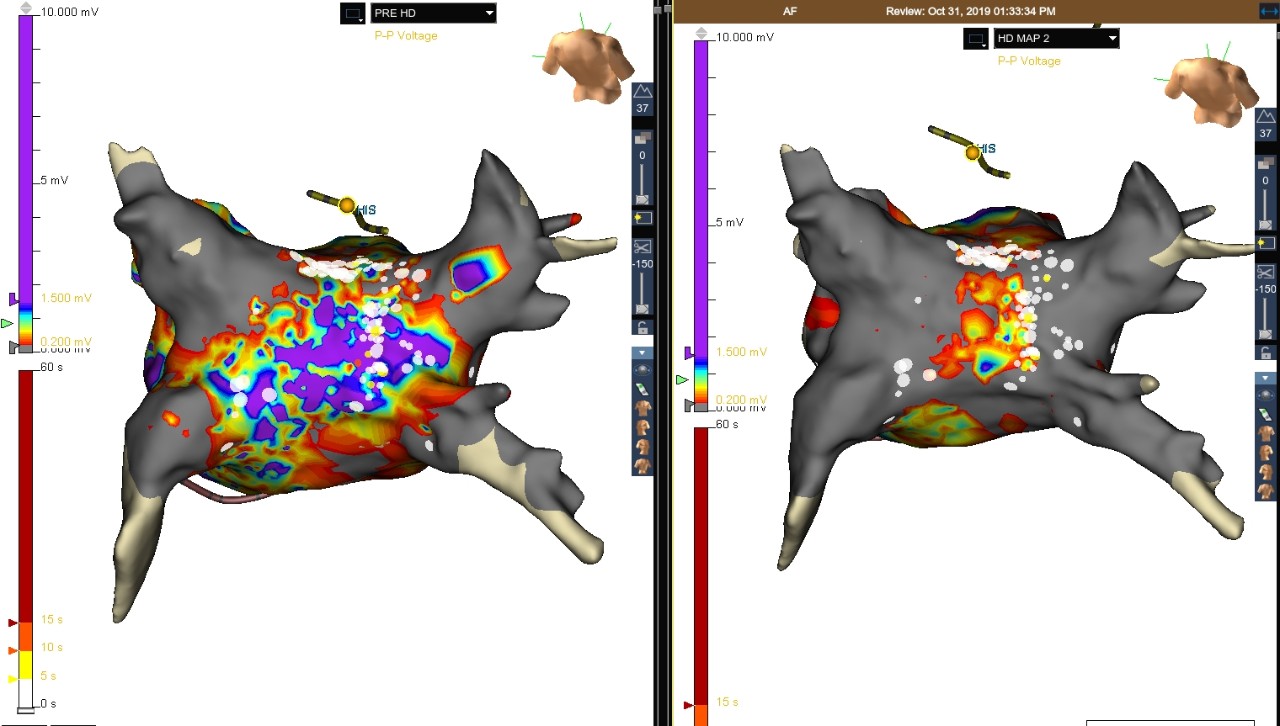
Voltage Map (Left) and Posterior Isolation of Right Veins RF Ablation (Right)
Post-Ablation Restored to NSR
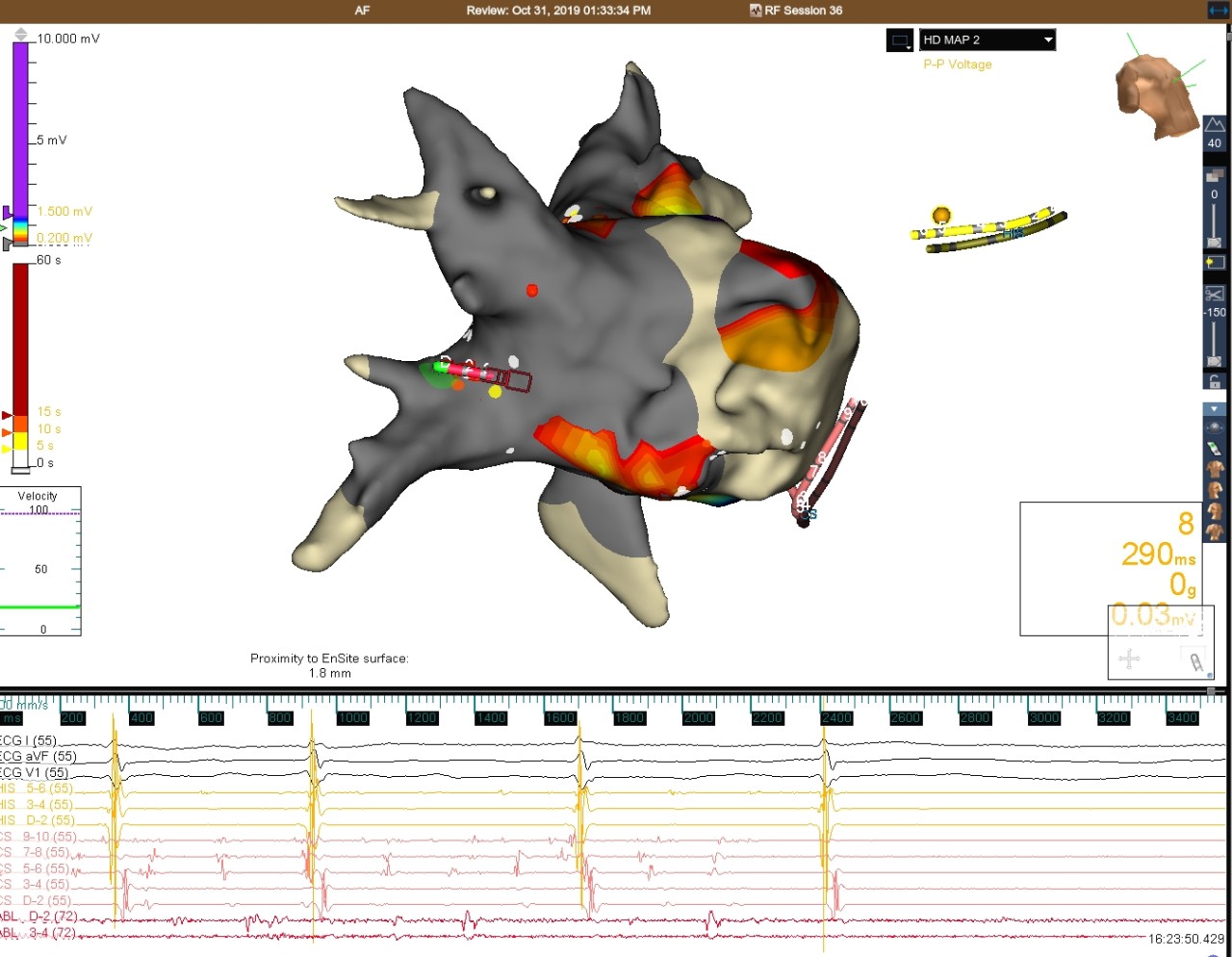
Atrial Fibrillation
This patient presented in persistent AFib for a cryoballoon PVI. After four unsuccessful cardioversions post ablation, the Advisor HD Grid Mapping Catheter, SE was used to create a voltage map. The roof and right veins were still active, so a roof line and posterior isolation of right veins was performed with RF ablation. Patient was still in AFib. A signal of 0.03 mV was picked up on the Advisor HD Grid Mapping Catheter, SE in the right carina, possibly from epicardial fibers. Upon ablation, the patient had a 12 sec conversion pause and restored to NSR.
Image courtesy of Dr. David Kenigsberg (Westside Regional Medical Center | Plantation, FL)
Reentrant LAT Map of the LA
Left Atrial Atypical Flutter
This case shows a patient with a prior PVI who presented in atypical atrial flutter. Entrainment revealed the rhythm was most likely left atrial dependent. The Advisor HD Grid Mapping Catheter, SE was used to create a reentrant LAT map of the LA, and the critical isthmus was revealed on the anterior wall.
Image courtesy of Dr. Farhat Khairallah (Tallahassee Memorial Healthcare | Tallahassee, FL)
Reentrant LAT Map of the LA
Left Atrial Atypical Flutter
This case shows a patient with left atrial atypical flutter who underwent a previous AFib ablation with no prior posterior wall ablation. The Advisor HD Grid Mapping Catheter, SE was used to create a reentrant LAT map of the LA. The flutter terminated after anchoring the existing line of block (black line) to the LIPV.
Image courtesy of Dr. Bohuslav Finta (Lutheran Medical Center | Wheat Ridge, CO)
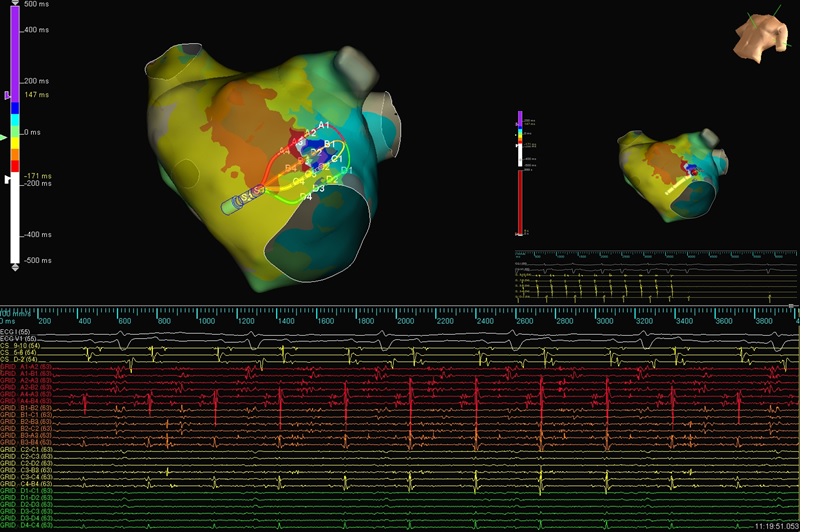
Atypical AFL & AT
Atypical AFL & AT
This case shows a patient who had a prior cryoablation PVI. Using Advisor HD Grid (assumption), two maps were created to reveal a double loop reentry atrial flutter and a focal tachycardia with the same cycle length.
Image courtesy of Dr. Abdul Alawwa (McLaren Regional Medical Center | Flint, MI)
Reentrant LAT Map of the LA
Left Atrial Antero-Septal Atypical Flutter
This case shows a patient with left atrial atypical flutter. The Advisor HD Grid Mapping Catheter, SE was used to create a reentrant LAT map of the LA, and the critical isthmus was revealed at the antero-septal aspect location.
Image courtesy of Dr. Rod Passman (Northwestern Memorial Hospital | Chicago, IL)
LAT Map of the LA
Left Atrial Microreentrant Tachycardia
This case shows a patient who presented with incessant tachycardia after two prior PVI ablations. The Advisor HD Grid Mapping Catheter, SE was used to create an LAT map of the LA, which revealed a microreentrant circuit on the anterior wall of the LA. The tachycardia was terminated with the first RF lesion, and NSR was restored in the patient.
Image courtesy of Dr. Jeffrey A. Olson (St. Vincent Hospital | Indianapolis, IN)
Redo Mitral Flutter
This case shows a patient who had a previous mitral isthmus line ablation. The patient presented in atrial flutter, and the Advisor HD Grid Mapping Catheter, SE was used to create a reentrant LAT map of the LA. SparkleMap was used to rapidly interpret the conduction dynamics of the circuit and to identify lines of block. SparkleMap helped to identify a critical deceleration zone (circled in yellow), which was a gap in the original lesion set.
The flutter terminated with RF ablation in the deceleration zone (orange lesion), starting at the mitral annulus and pulling back through the gap to anchor the lesion set to scar.
Image courtesy of Dr. Shaun Cho (El Camino Hospital | Palo Alto, CA)
LAT Map of the RA
Atypical AFL
In this case, the patient presented to the EP lab in tachycardia and the Advisor HD Grid Mapping Catheter, SE was used to create a map of the right atrium. Reentrant LAT map demonstrated that the rhythm was upper loop reentry atrial flutter. High density mapping also revealed the conduction of a smaller loop into and out of the SVC, with collision with the dominant wavefront medial to the right atrial appendage. The atrial flutter was terminated with a linear lesion set connecting an SVC line of block to the IVC.
Image courtesy of Dr. Azlan Hussin (Institut Jantung Negara - The National Heart Institute | Kuala Lumpur, Malaysia)
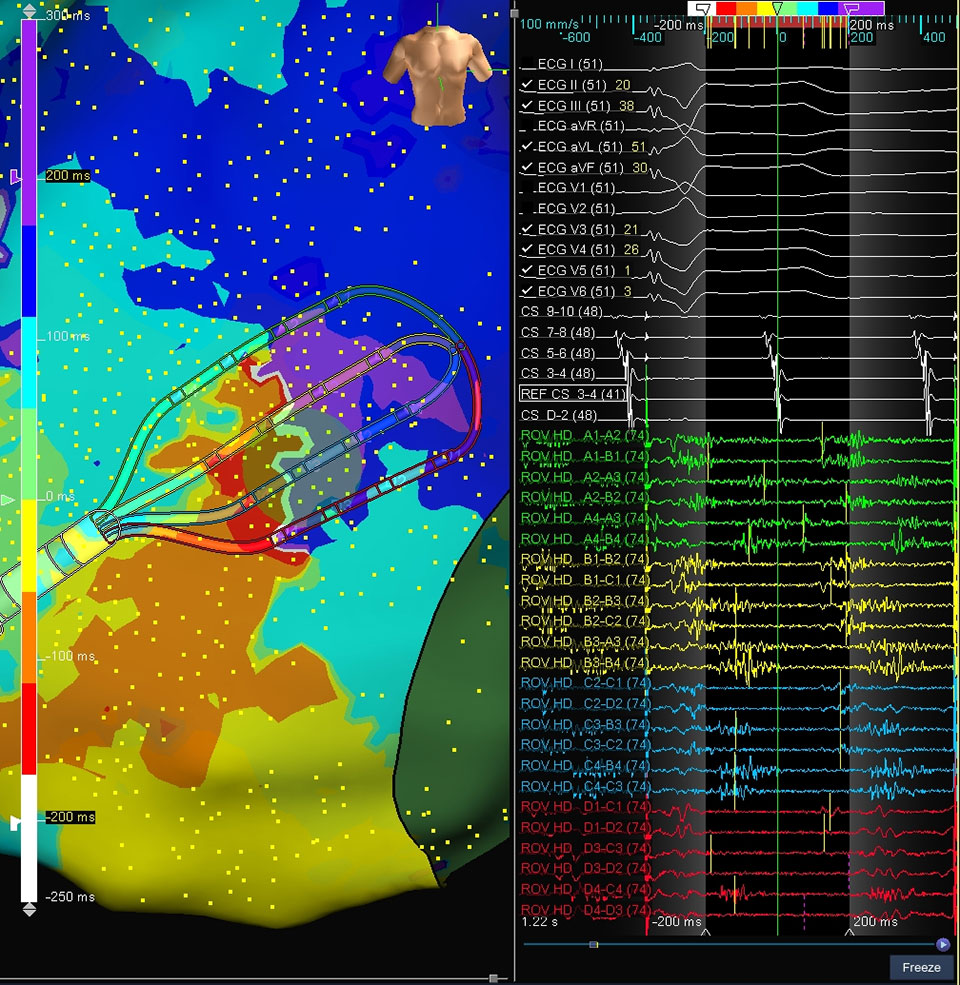
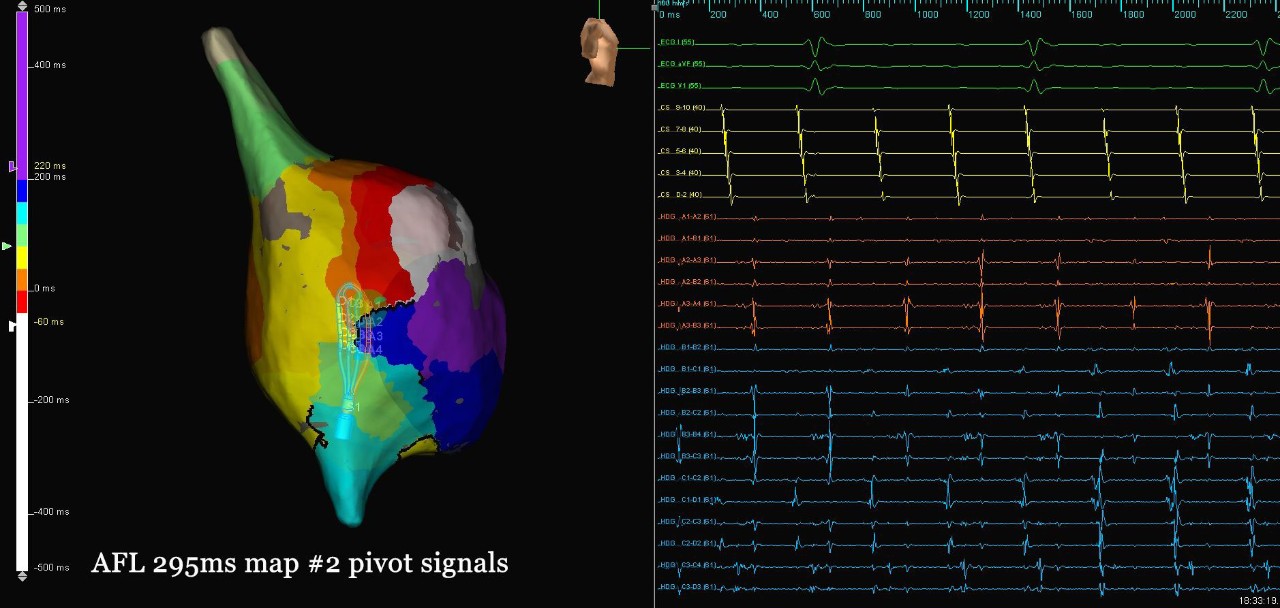
Micro Reentry Signals
Atypical AFL
In this case, the patient presented to the EP lab following a prior focal atrial tachycardia and CTI ablation. A high-density map of the right atrium was created using the Advisor HD Grid Mapping Catheter, SE, and it revealed a micro-reentrant atrial flutter in the lateral wall pivoting around a single line of block. The unique design of the HD Grid allowed for the visualization of the entire circuit within the catheter’s EGMs when placed adjacent to the line of block. Ablation between the line of block and the tricuspid valve annulus terminated the flutter.
Image courtesy of Dr. Eric Lim (National Heart Center | Singapore)
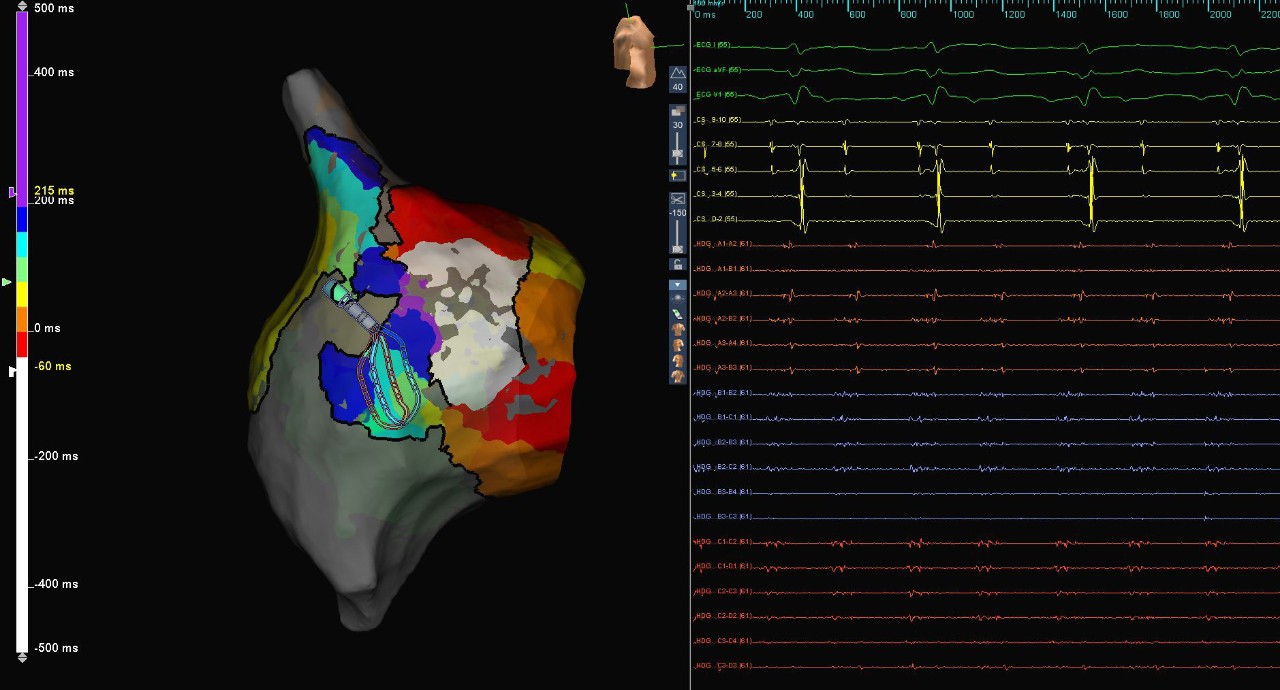
Map of AFL Right Ventricle
Atypical AFL
This patient presented in atrial flutter following prior cardiac surgery and cavo-tricuspid isthmus ablation. High-density mapping using the Advisor HD Grid Mapping Catheter, SE helped to identify the flutter circuit rotating around a line of block on the lateral wall of the right atrium. The flutter terminated during the first lesion at the more posterior pivot point along the line of block; an additional lesion set was created to anchor the line of block to the IVC. Additionally, a line of block with was seen along the entire duration of the CTI, suggesting durable CTI block.
Image courtesy of Dr. Eric Lim (National Heart Center | Singapore)
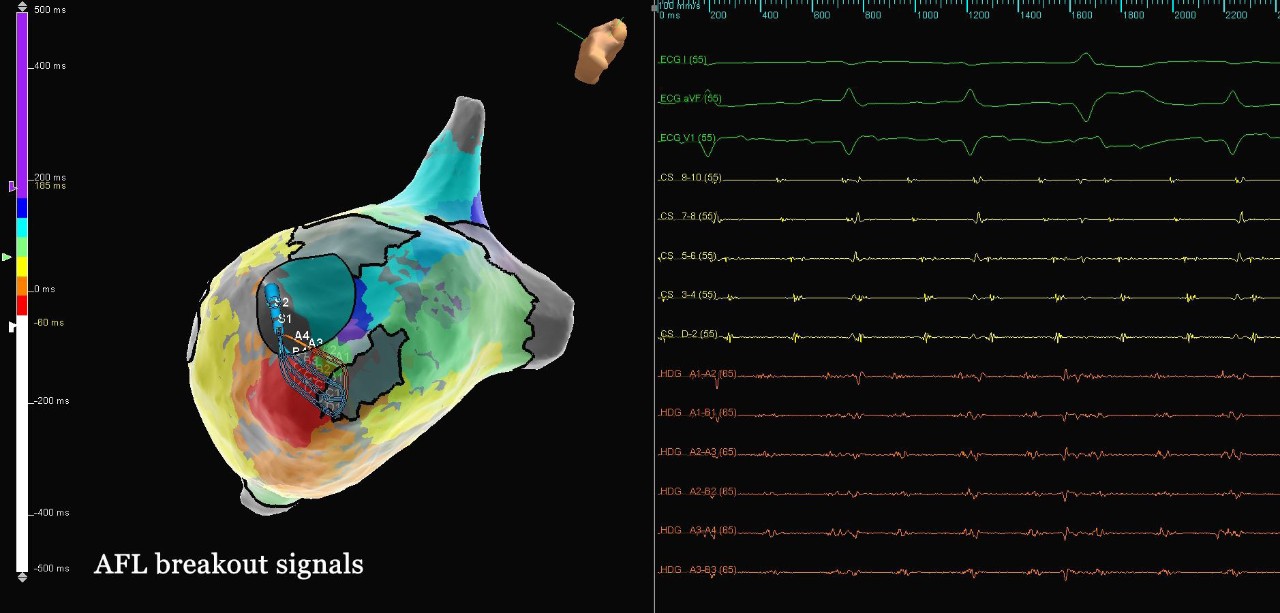
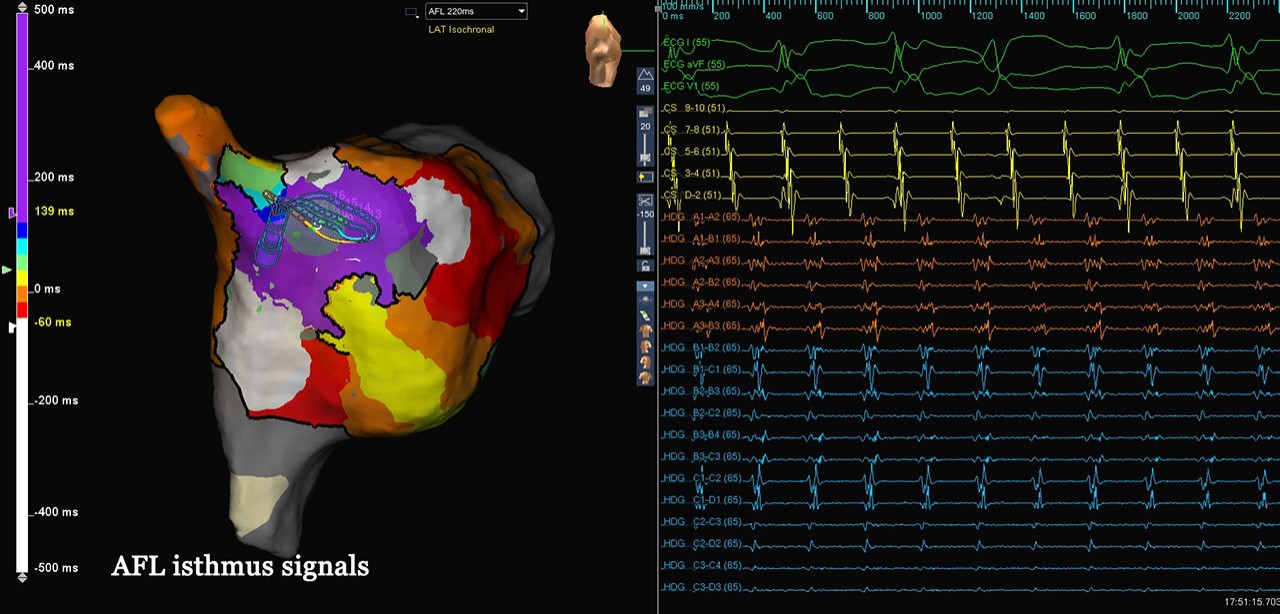
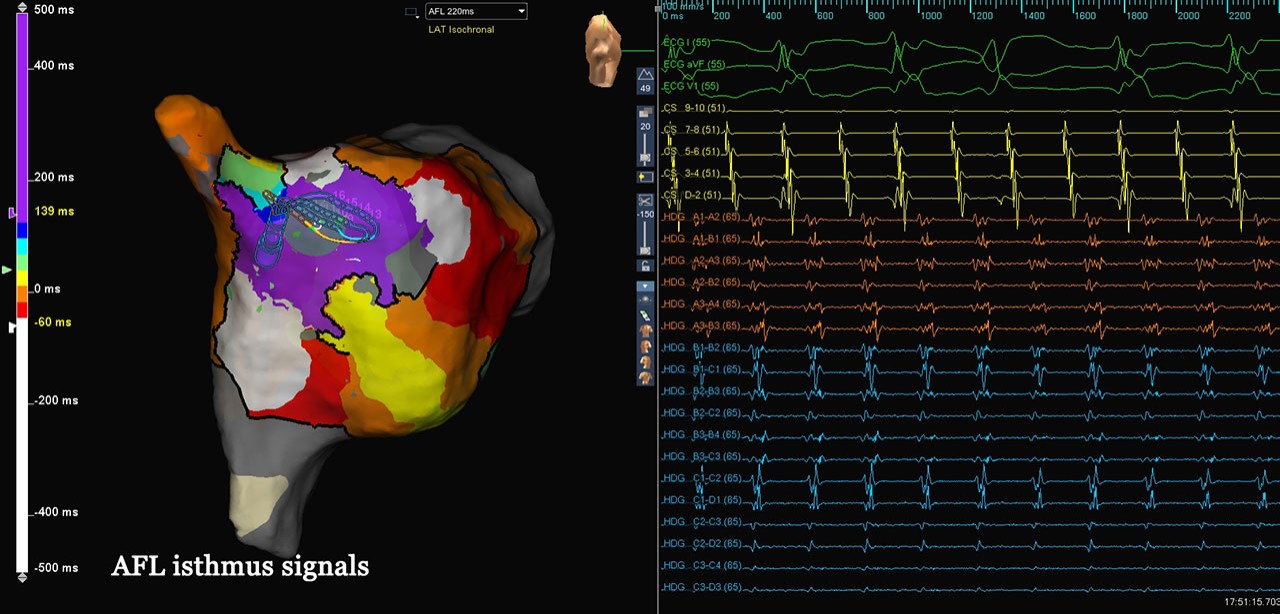
AFL Isthmus Signals
Atypical AFL
In this case, the patient presented to the EP lab with a history of severe tricuspid regurgitation and tricuspid valve replacement, as well as a prior cavo-tricuspid isthmus ablation. A high-density map of the right atrium was created using the Advisor HD Grid Mapping Catheter, SE, revealing areas of slow conduction, wavefront collision, and complex lines of block along the lateral wall. While the HD Grid Catheter was in good contact with the lateral wall, it displayed complex fractionated electrograms throughout the diastolic window.
Image courtesy of Dr. Tan Vern Hsen (Changi General Hospital | Singapore)
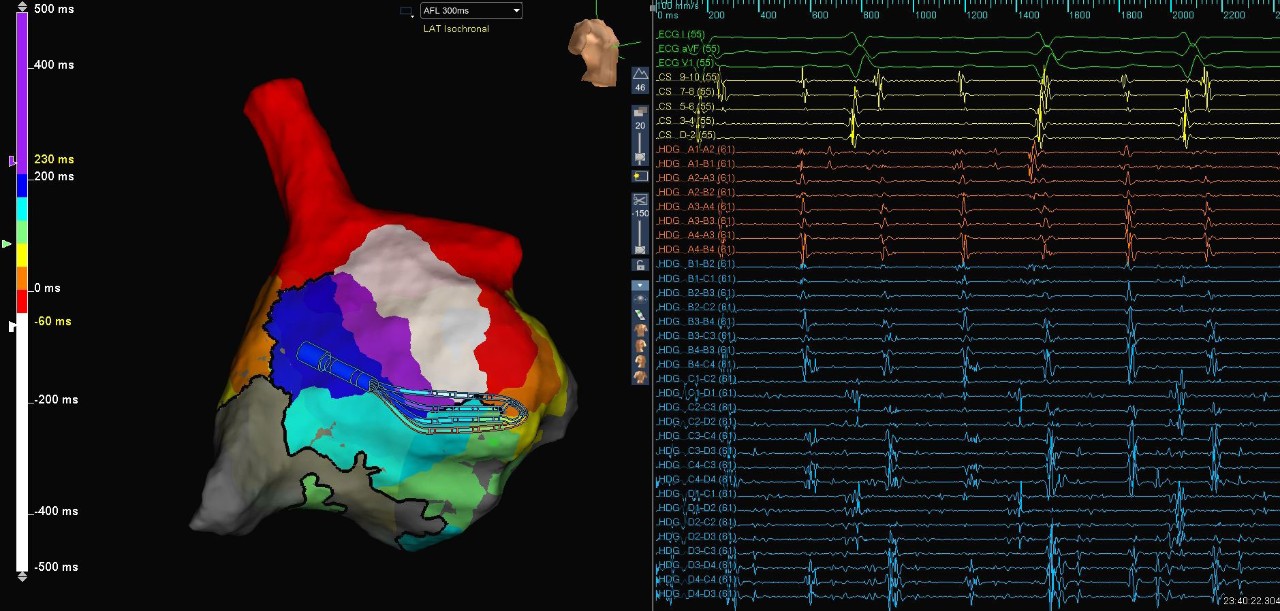
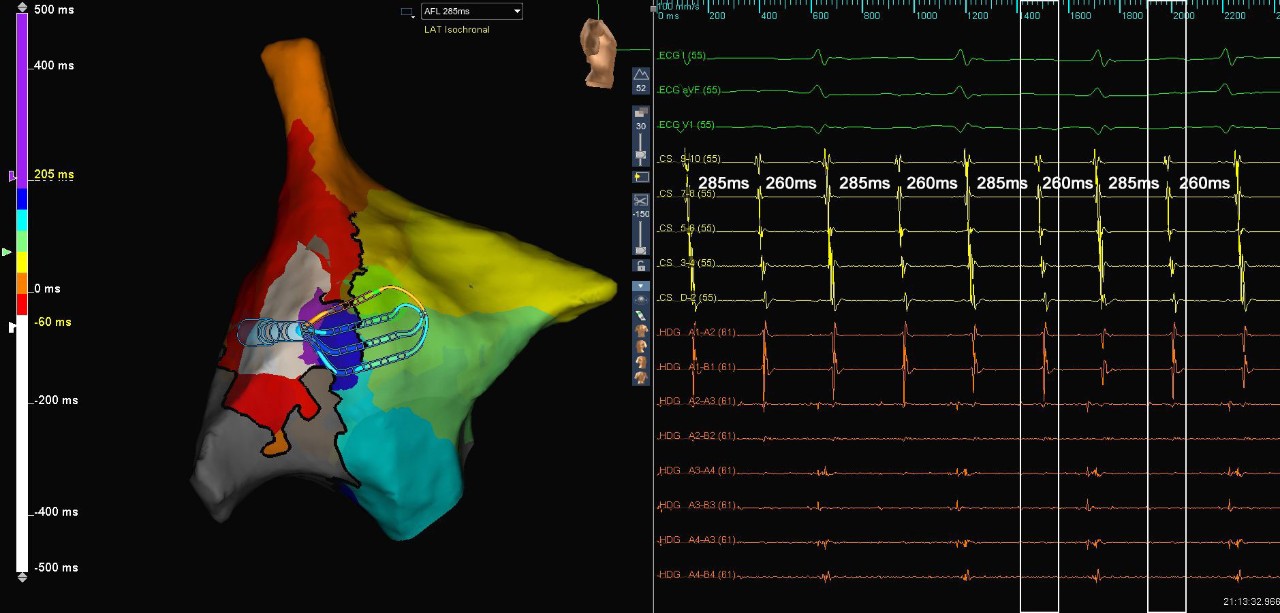
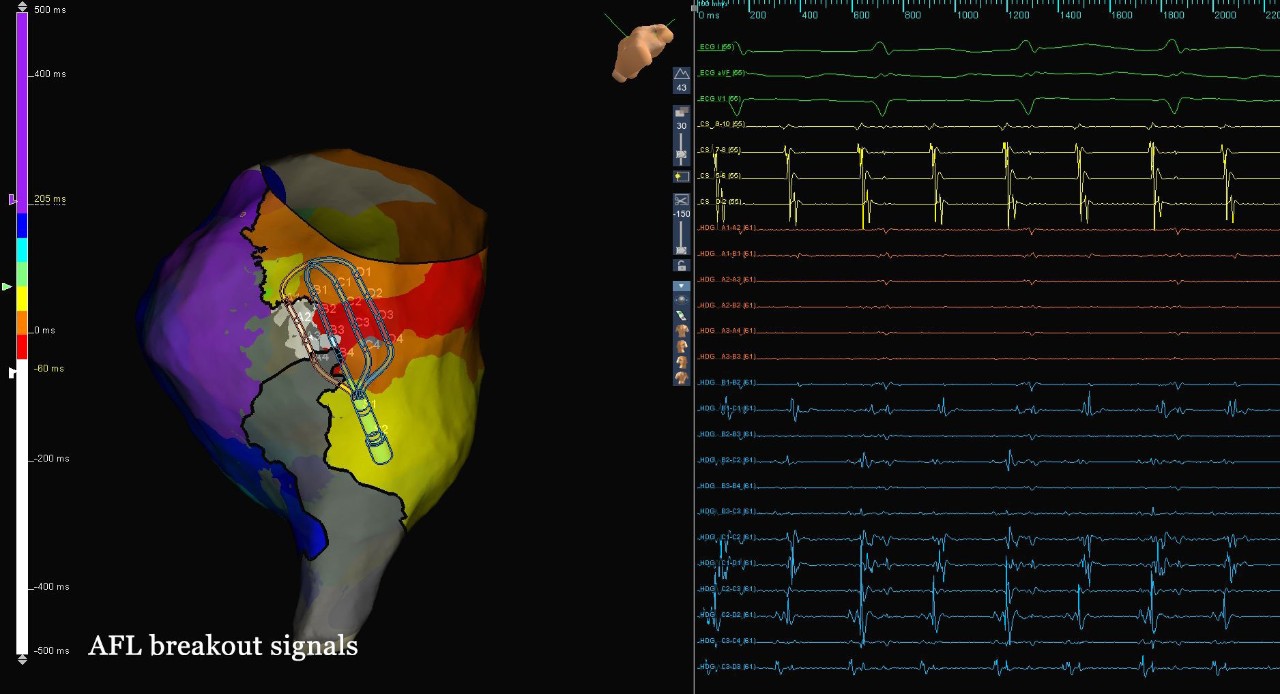
Map of AFL Isthmus Signals
Atypical AFL
This patient presented in atrial flutter subsequent to cavo-tricuspid isthmus ablation and tricuspid valve replacement. The right atrium was mapped with the Advisor HD Grid Mapping Catheter, SE, revealing a microreentrant circuit and a critical site of slow conduction along the anterior portion of the SVC-RA junction. High-density mapping of the critical isthmus exit site displayed a complex breakout pattern, with multiple wavefronts wrapping around lines of block and colliding with each other. A single ablation at the critical isthmus entrance site terminated the rhythm.
Image courtesy of Dr. Azlan Hussin (Institut Jantung Negara - The National Heart Institute | Kuala Lumpur, Malaysia)
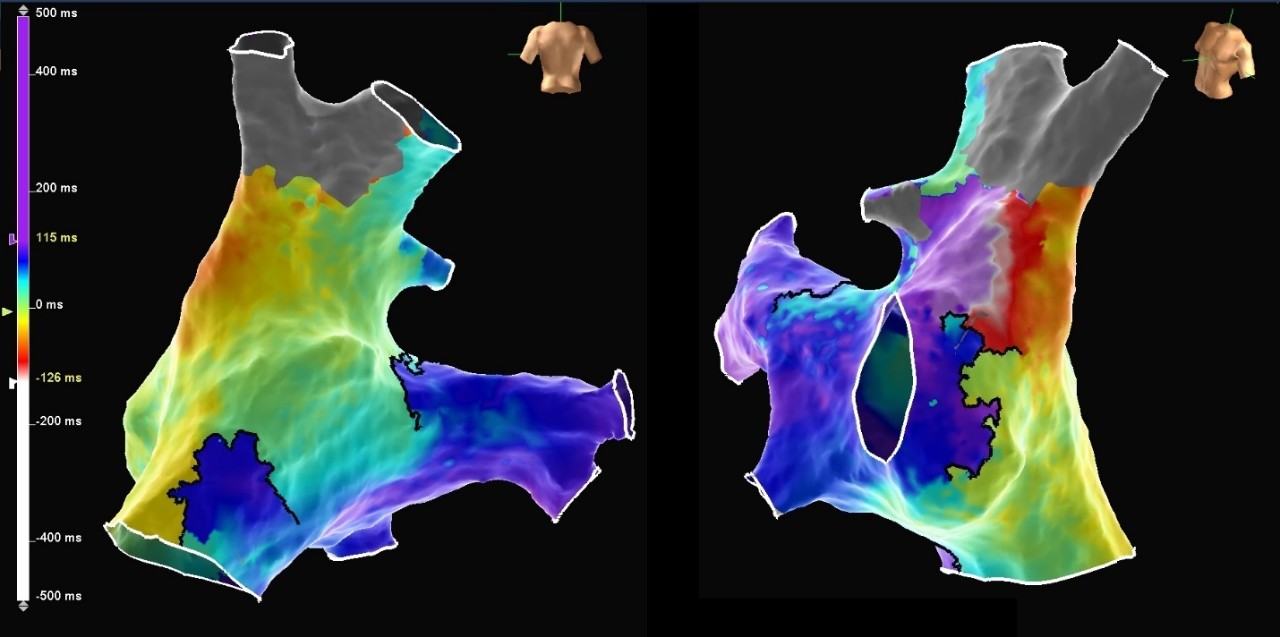
Map of AFL Right Ventricle
Atypical AFL
In this case, the patient presented in atrial flutter with cycle length alternans between 260 ms and 285 ms. A map of the right atrium was created using the Advisor HD Grid Mapping Catheter, SE and the AutoMap Module set up to selectively collect points only during the faster cycle length. Following this initial interrogation of the chamber, an additional map was created of the slower cycle length using TurboMap and the recording of the initial interrogation, and the maps were compared to understand the mechanism of the alternans. The faster cycle length correlated with a microreentrant circuit in the posterolateral right atrium, while the slower cycle length was attributed to a macroreentrant circuit along the lateral wall with unidirectional conduction through the region of microreentry.
Image courtesy of Dr. Azlan Hussin (Institut Jantung Negara - The National Heart Institute | Kuala Lumpur, Malaysia)
CTI Gap Signals
Typical AFL
This patient presented to the EP Lab in atrial flutter with a history of prior cavo-tricuspid isthmus ablation. A map of the right atrium was created using the Advisor HD Grid Mapping Catheter, SE, revealing a gap in the prior CTI line. A single ablation at this site closed the gap and terminated atrial flutter, leading to bidirectional block across the CTI.
Image courtesy of Dr. Eric Lim (National Heart Center | Singapore)
IART in Fontan Situs Inversus
The Advisor HD Grid Mapping Catheter, Sensor Enabled allowed precise visualization of the macro-reentrant arrhythmia circuit even in the regions of very low voltage. The unusual anatomy after the Fontan cardiac surgical repair and situs inversus was not an issue, and the Advisor HD Grid Mapping Catheter, Sensor Enabled was able to assist in creating a detailed, CT-like model to aid in visualization of the chamber.
Image courtesy of Dr. Környei László (Hungarian Pediatric Heart Center | Budapest, Hungary)
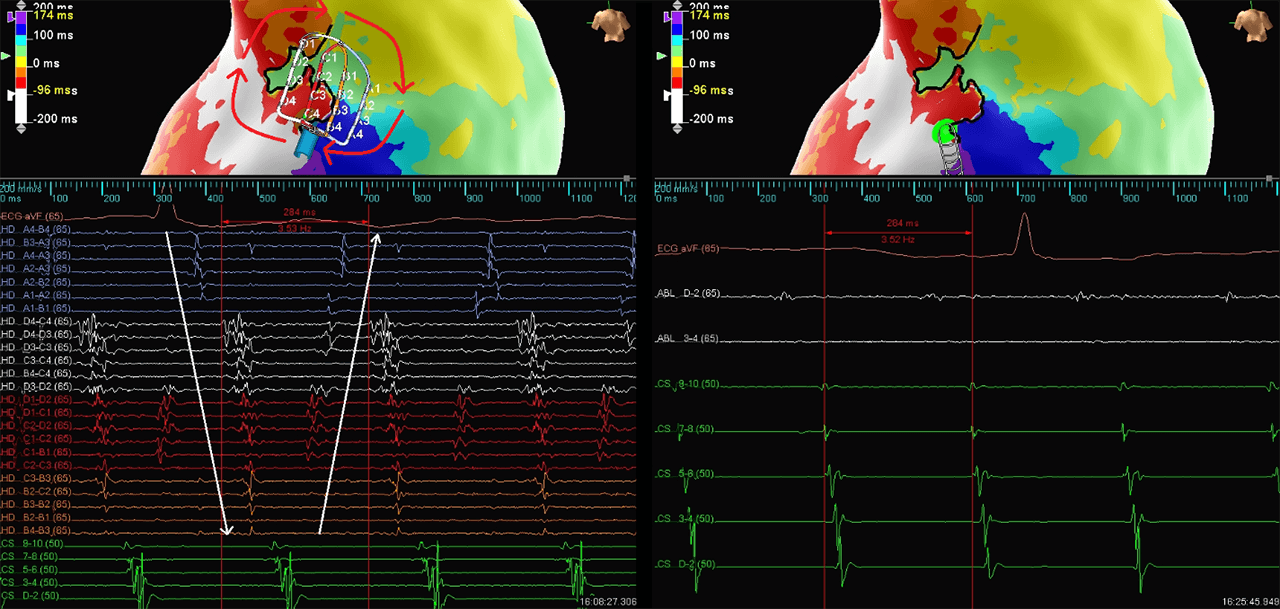
Atypical Flutter
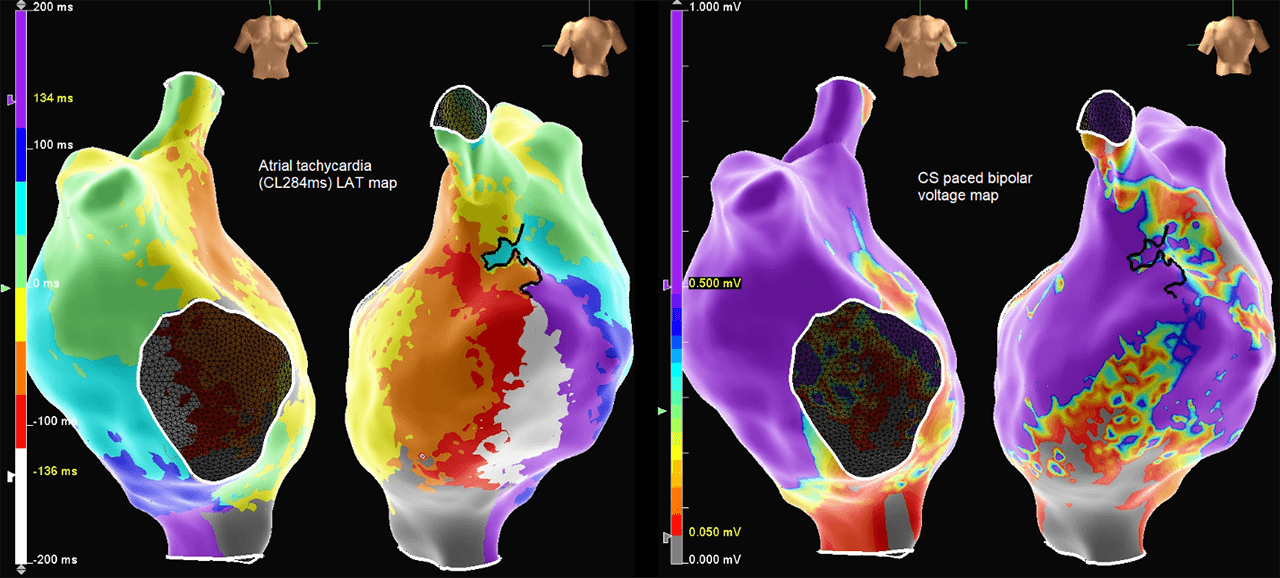
HD voltage and LAT maps
Redo CTI
Despite previous suspicions that this would be a redo CTI ablation, the CTI line was identified as intact. Atrial tachycardia (CL284ms) was induced and mapped with the Advisor HD Grid Mapping Catheter, Sensor Enabled using the abs dVdT detection algorithm. The entire cycle length of the atypical flutter was observed below. Equivalent EGMs were not observed on the ablation catheter when positioned at the same location as the Advisor HD Grid Mapping Catheter, Sensor Enabled. Analysis of the HD voltage and LAT maps allowed for quick and accurate identification of the isthmus. Minimal ablation lesions were required to terminate flutter. The Advisor HD Grid Mapping Catheter, Sensor Enabled provided important information, which allowed for improved safety through reduced ablation and procedure time.
Image courtesy of Dr. Damian P. Redfeam (Kingston Health Sciences Centre | Ontario, Canada)
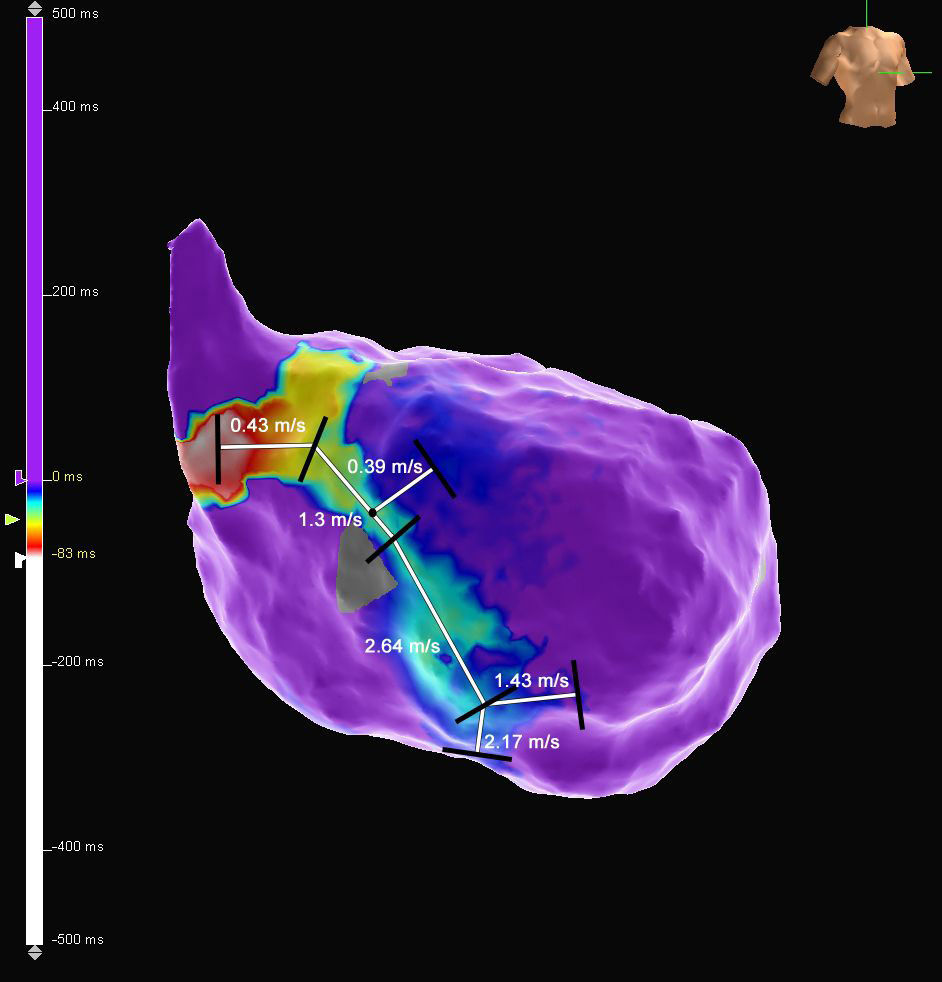
RA Right Lateral AP
RA Right Lateral AP
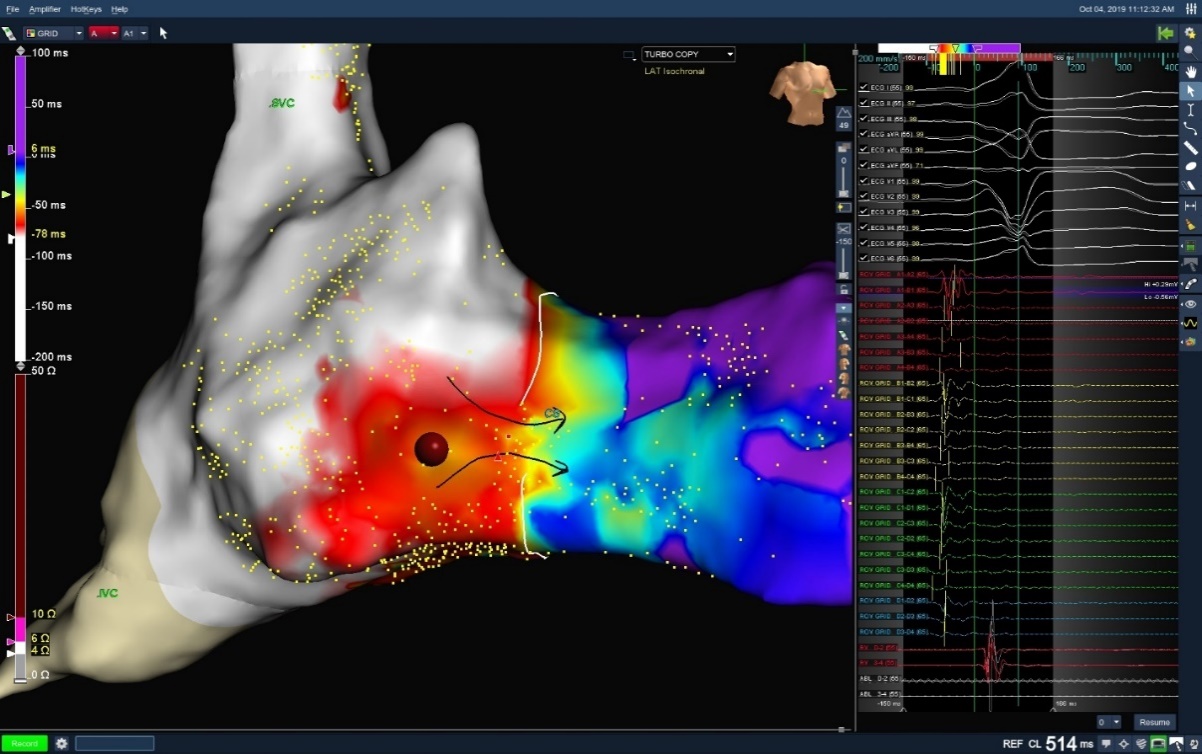
RA Right Lateral Accessory Pathway
Using the Advisor HD Grid Mapping Catheter, Sensor Enabled to perform the open window mapping technique, a right lateral accessory pathway was identified. Precise localization of the accessory pathway allowed for successful ablation, noted by the elimination of pre-excitation within two seconds of the first RF lesion. Below is a demonstration of open window mapping of RA Right Lateral AP with the Advisor HD Grid Mapping Catheter, Sensor Enabled. Pre-excitation was eliminated with two seconds on one burn.
Image courtesy of Dr. John P. McKenzie, III (Glendale Memorial Hospital | Glendale, CA)
LAT Map Showing Point Density - RA
LAT Map of the RA: Right Atrial Focal AT
Right Atrial Focal AT
This case shows a patient who presented with AT. During pulmonary vein isolation (PVI) ablation, the Advisor HD Grid Mapping Catheter, SE was used to create an LAT map of the LA. The LAT map showed the AT was originating from the RA. The Advisor HD Grid Mapping Catheter, SE was then used to create an LAT map of the RA, which showed the earliest activation at the mid-lateral location of the RA. The focal AT was terminated with the first RF lesion, and NSR was restored in the patient.
Image courtesy of Dr. Steven Fowler (Community Hospital of the Monterey Peninsula | Monterey, CA)
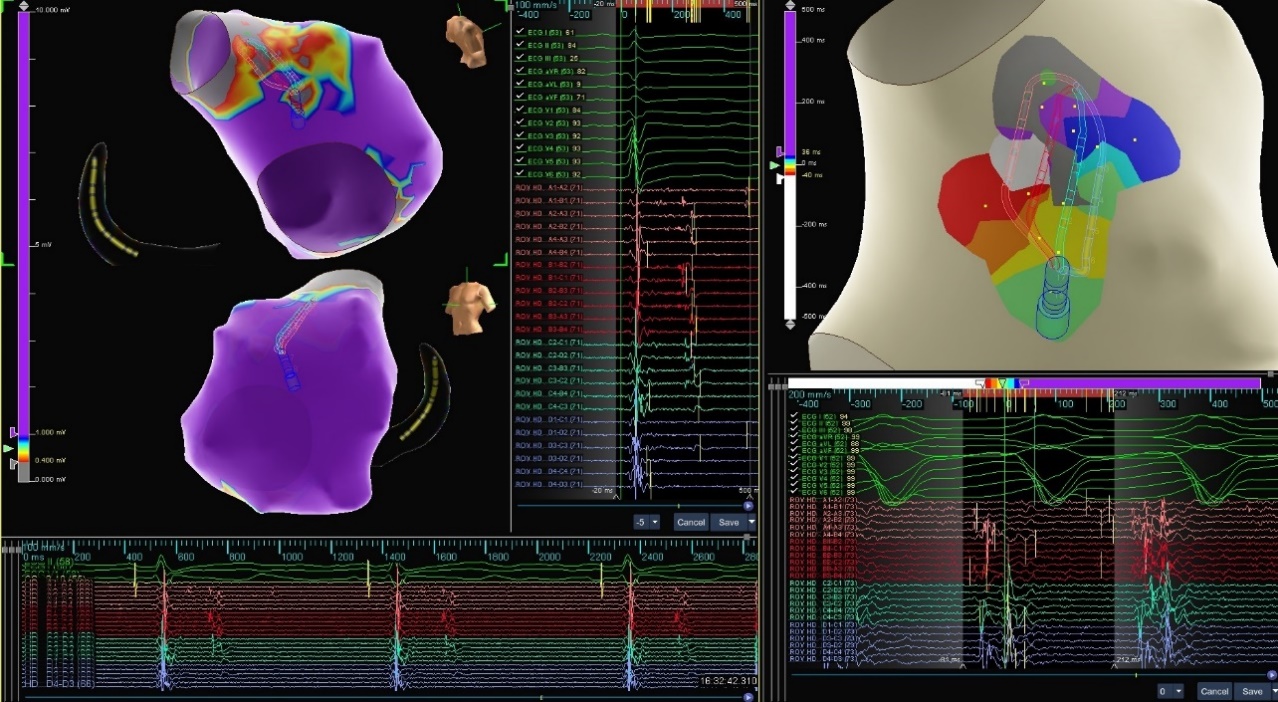
First Deflection Fascicle Map
Ischemic VT
This patient presented to the EP lab following recurrent episodes of ventricular tachycardia from a prior myocardial infarction. An isochronal late activation map of the left ventricle was created using the Advisor HD Grid Mapping Catheter, SE and the Last Deflection algorithm to automatically annotate abnormal and late ventricular activation. This map displayed an area of slowing and late potentials along the left ventricular septal wall near the area of the posterior fascicle. To more clearly define the posterior fascicle prior to ablation, the recording of the initial interrogation of the chamber with the HD Grid was loaded and an additional map was created using the TurboMap and First Deflection algorithms to efficiently annotate the earliest signal.
Image courtesy of Dr. Eric Lim (National Heart Center | Singapore)
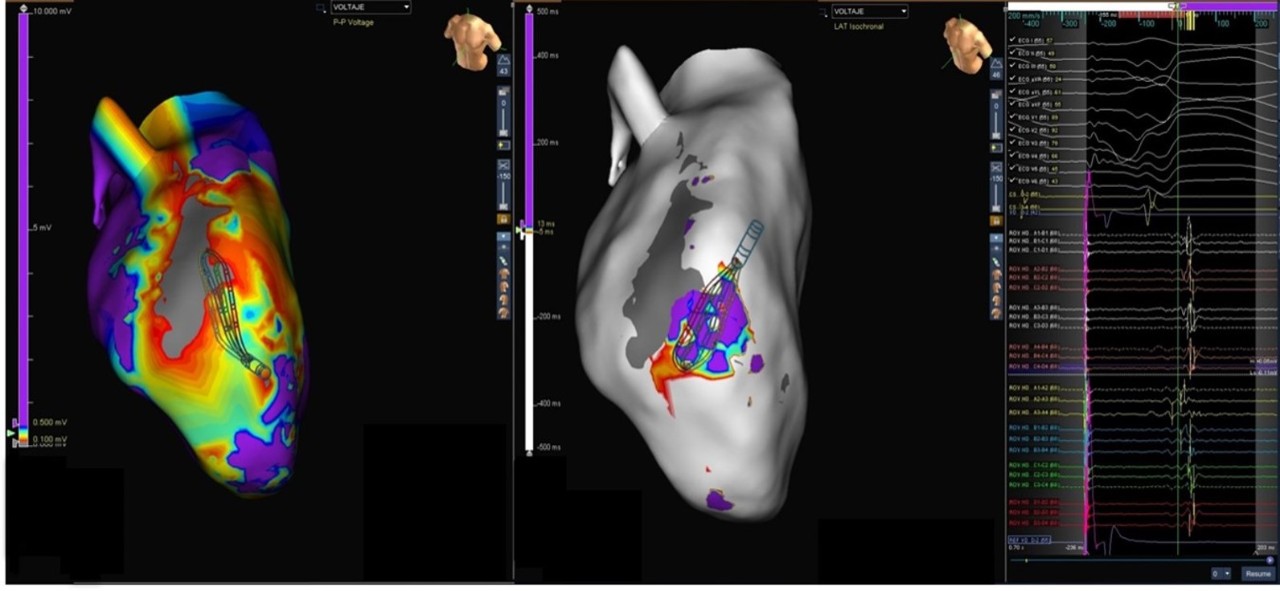
VT Ablation
Presented here is a figure eight VT circuit identified in a patient with anterior infarct. The Advisor HD Grid Mapping Catheter, Sensor Enabled allowed for precise mapping and visualization of the circuit’s critical isthmus. VT was terminated within 11 seconds of the first lesion and was no longer inducible.
Image courtesy of Dr. Ricardo Salgado Aranda (University Hospital of Burgos | Burgos, Spain)
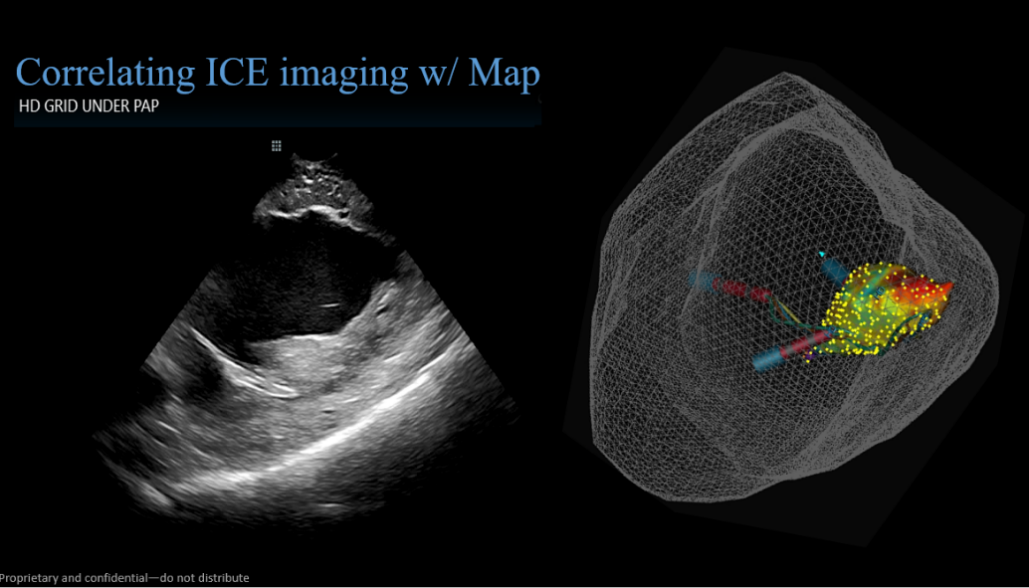
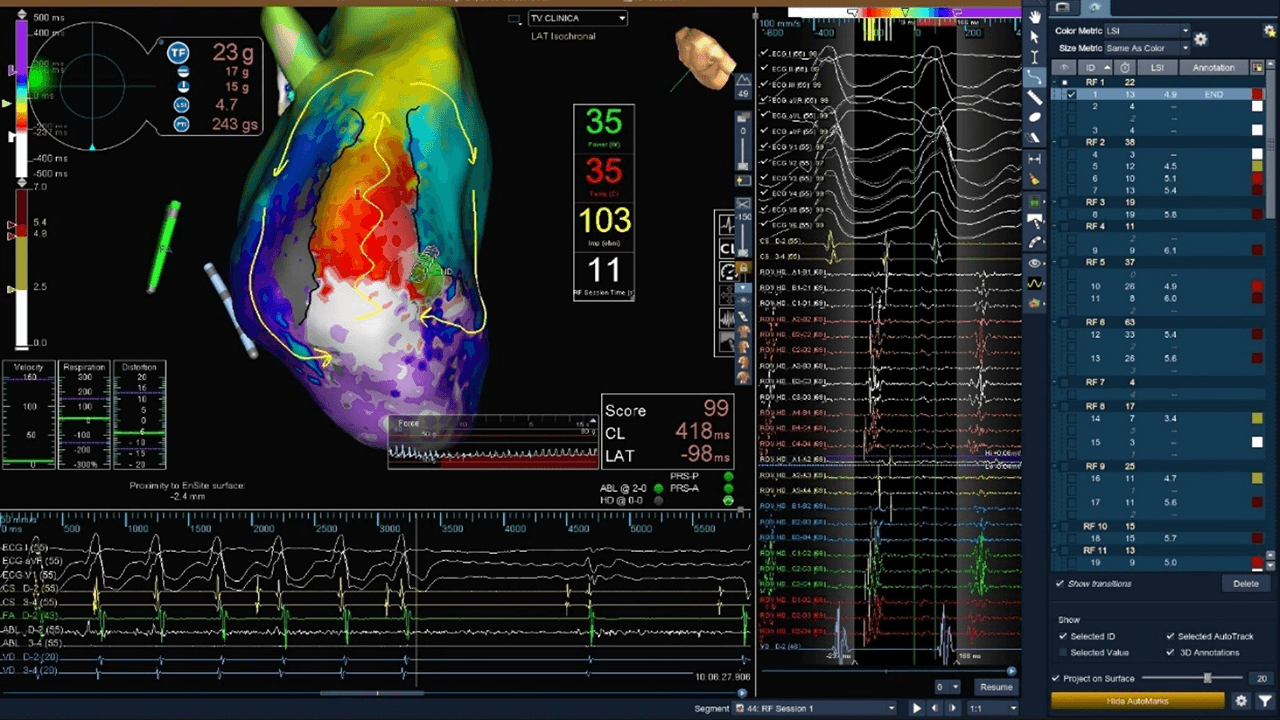
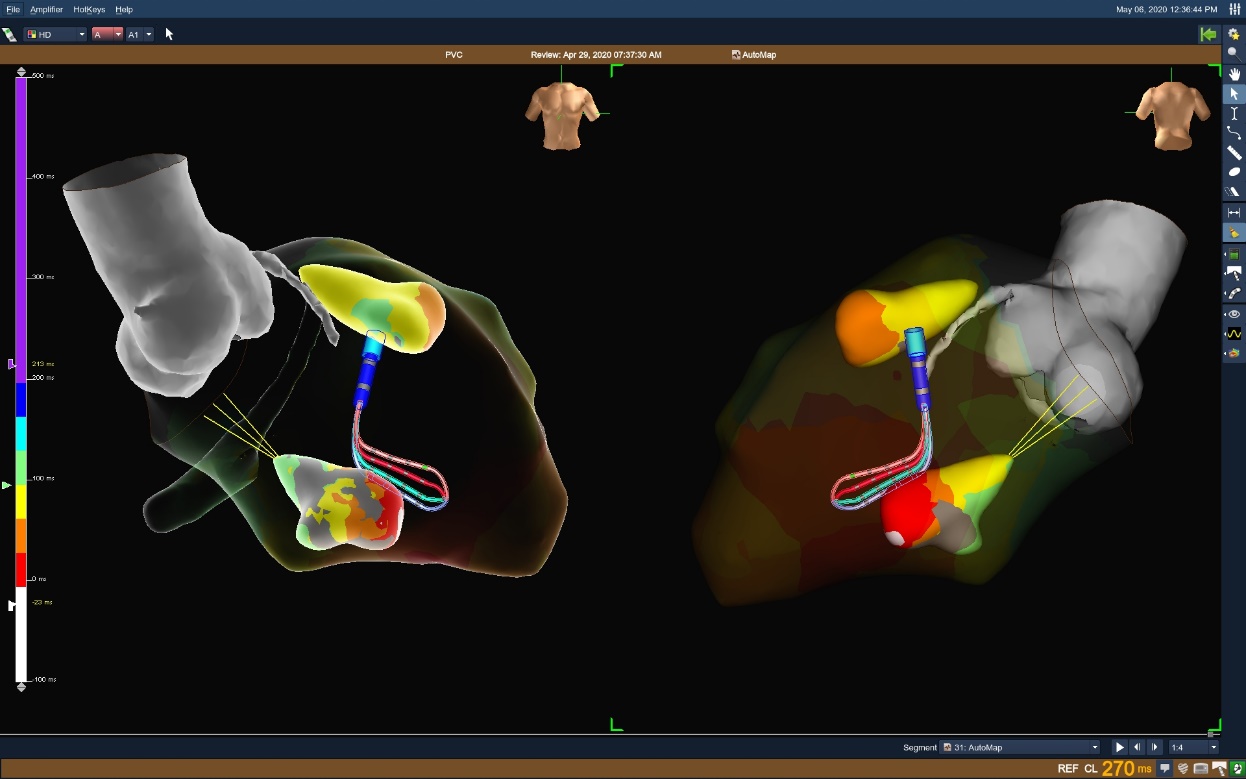
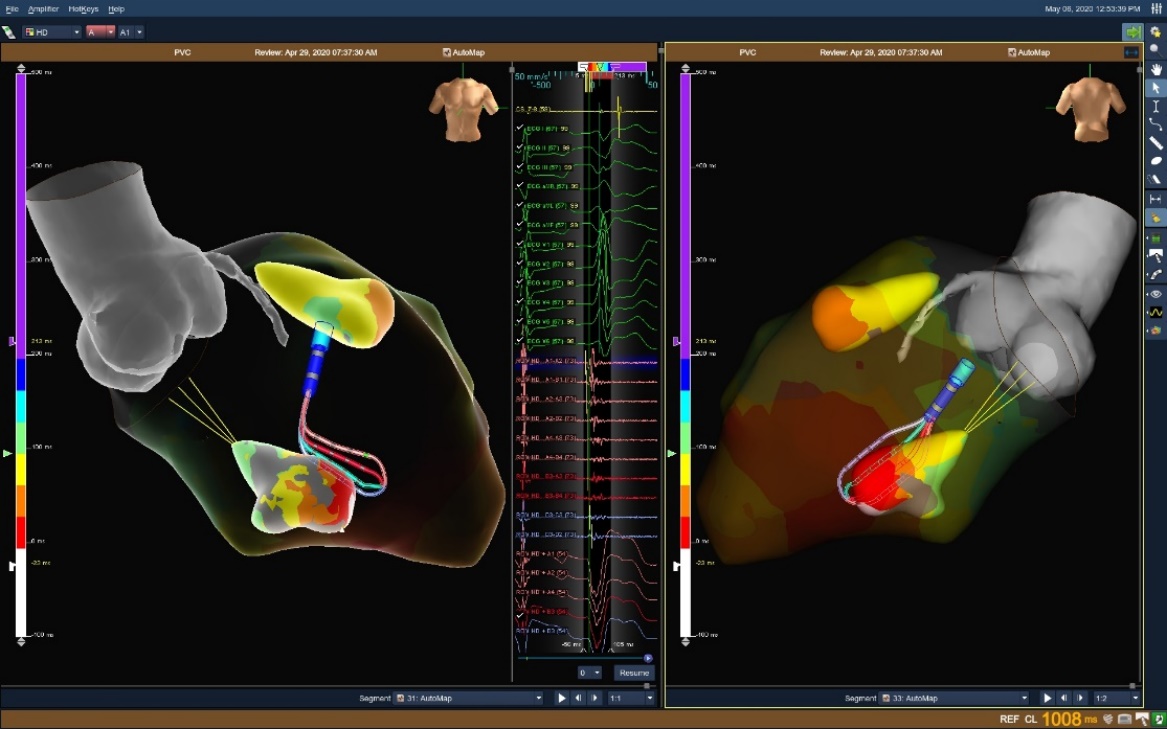
PVC
Advisor HD Grid Mapping Catheter, Sensor Enabled was instrumental in creating a High Density map of the LV quickly and efficiently to localize bigeminal PVCs. While carefully correlating the location of the papillary muscles with Viewmate™ ICE, the Advisor HD Grid Mapping Catheter, Sensor Enabled, maneuvered seamlessly underneath and around the papillary muscles, making localization of fractionated PVC focus obvious. RF ablation was delivered at the base of the anterior papillary muscle, resulting in acceleration and termination of the PVCs. The patient’s PVC-induced cardiomyopathy continued to improve as PVCs were eliminated.
Image courtesy of Dr. B. John Hynes (Deborah Heart and Ling Center | Brown Mills, NJ)
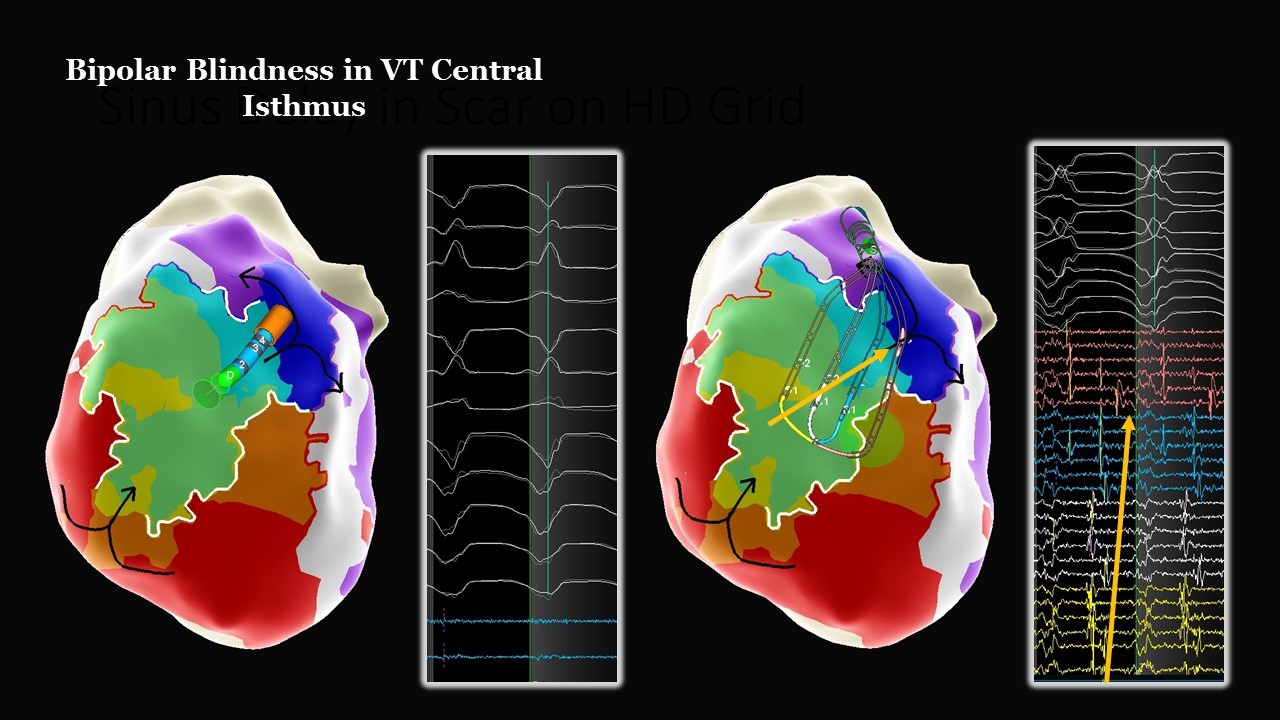
Bipolar Blindness in VT Central Isthmus
Ischemic VT
The Advisor HD Grid Mapping Catheter, Sensor Enabled allowed for quick identification of the central isthmus in this reentrant VT circuit. With the use of the Advisor HD Grid Mapping Catheter, Sensor Enabled the wavefront diagonal to the splines highlighted VT propagation from isthmus to exit. This wavefront was not visualized using the bipolar ablation catheter.
Image courtesy of Dr. John Wylie (St. Elizabeth's Medical Center | Brighton, MA)
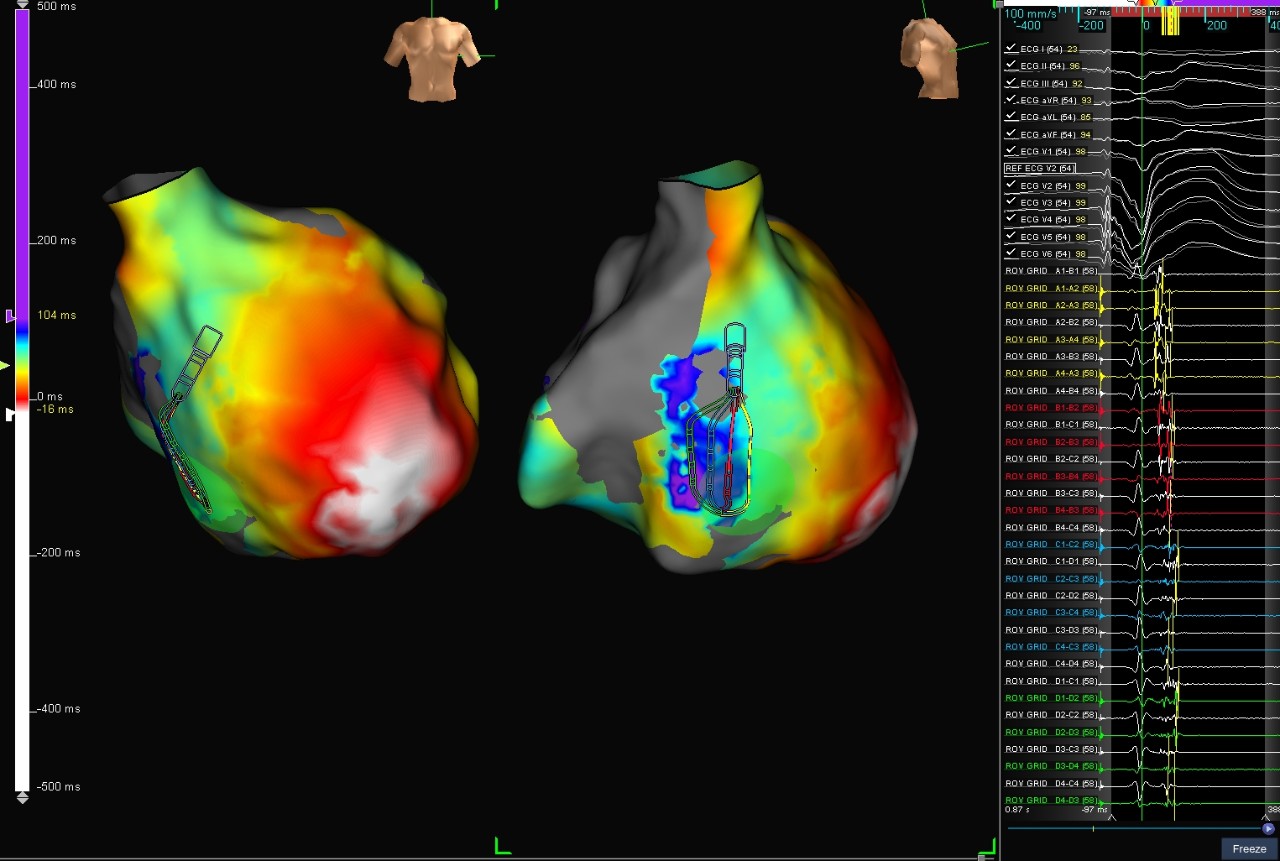
LV Papillary Muscle PVC
Patient had a two-year history of symptomatic palpitations. The Advisor HD Grid Mapping Catheter, Sensor Enabled was used to rapidly reconstruct the LV and papillary muscles while simultaneously collecting a local activation map utilizing the First Deflection algorithm and AutoMap. Advisor HD Grid Mapping Catheter, Sensor Enabled identified low voltage pre-systolic signals for a target location within ten minutes.
Image courtesy of Dr. Ashit Patel (Cascade Cardiology Group and Salem Health Hospital |Salem, OR)
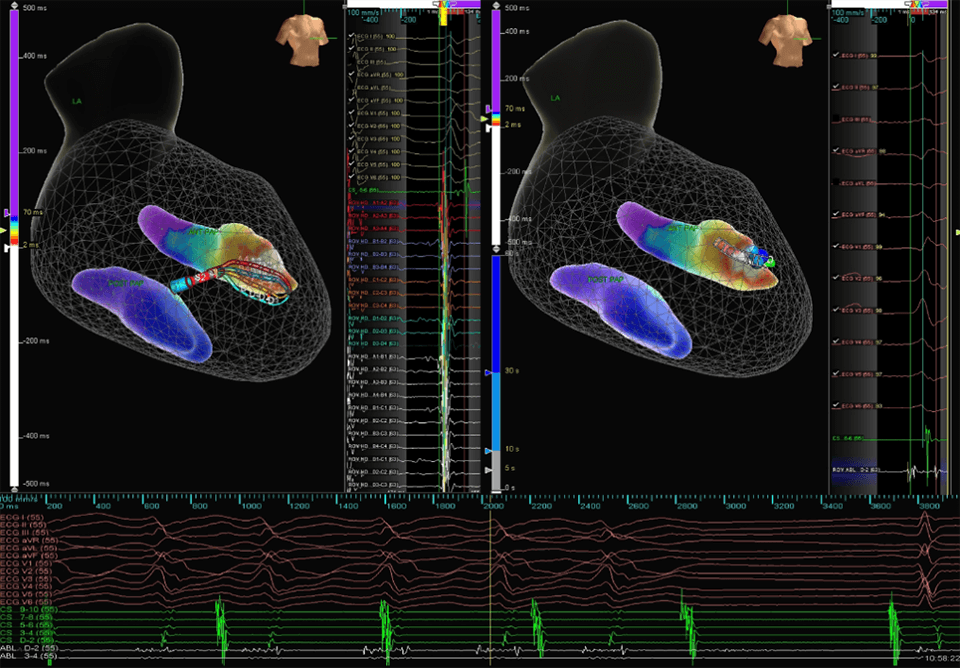
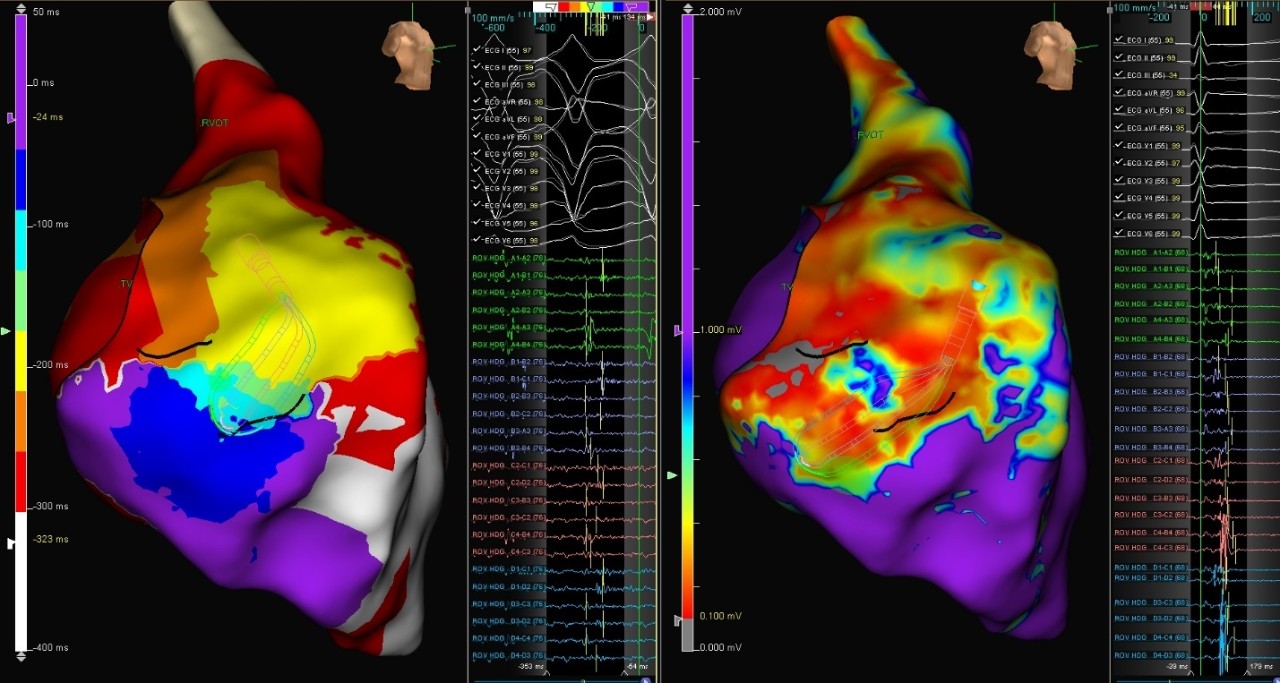
LAT Map with the Last Deflection Algorithm
Voltage Map
Ischemic VT
This case shows a patient with a CRT-D device and ischemic VT. With RV only pacing, the Advisor HD Grid Mapping Catheter, Sensor Enabled was used to create a local activation timing (LAT) map with the Last Deflection algorithm (left) and voltage map (right). The maps show local abnormal ventricular activities (LAVA) EGMs on the basal septum in the LAT map (left) correlating with a posterior voltage channel in the voltage map (right).
Image courtesy of Dr. John Nguyen (Mercy Hospital | Coon Rapids, MN)
Parahisian PVC
This Parahisian PVC was localized to just below the NCC with visual Advisor HD Grid Mapping Catheter, Sensor Enabled contact and higher amplitude signals down-the-spline. The clinical PCS was eliminated at the earliest site of activation.
Image courtesy of Dr. Alex Baher (Mercy Hospital | Coon Rapids, MN)
Redo VT
Patient was brought to the EP lab for Right Ventricle (RV) substrate evaluation after failed previous ablation attempt. The Advisor HD Grid Mapping Catheter, Sensor Enabled, with AutoMap and the last deflection detection algorithm revealed RVOT free-wall with fractionation and late potentials. A micro-reentrant circuit was found and confirmed with pacing.
Image courtesy of Dr. Randy Jones (Providence St. Vincent | Portland, Oregon)
NICM Redo RV VT
This patient with non-ischemic cardiomyopathy was presented with Right Ventricle (RV) VT. Using the Advisor HD Grid Mapping Catheter, Sensor Enabled, the deceleration zone was identified on the sinus rhythm, as visualized by the ILAM map. This was correlated with VT isthmus.
Image courtesy of Dr. Wendy S. Tzou (University of Colorado Hospital (UCH) | Aurora, CO)
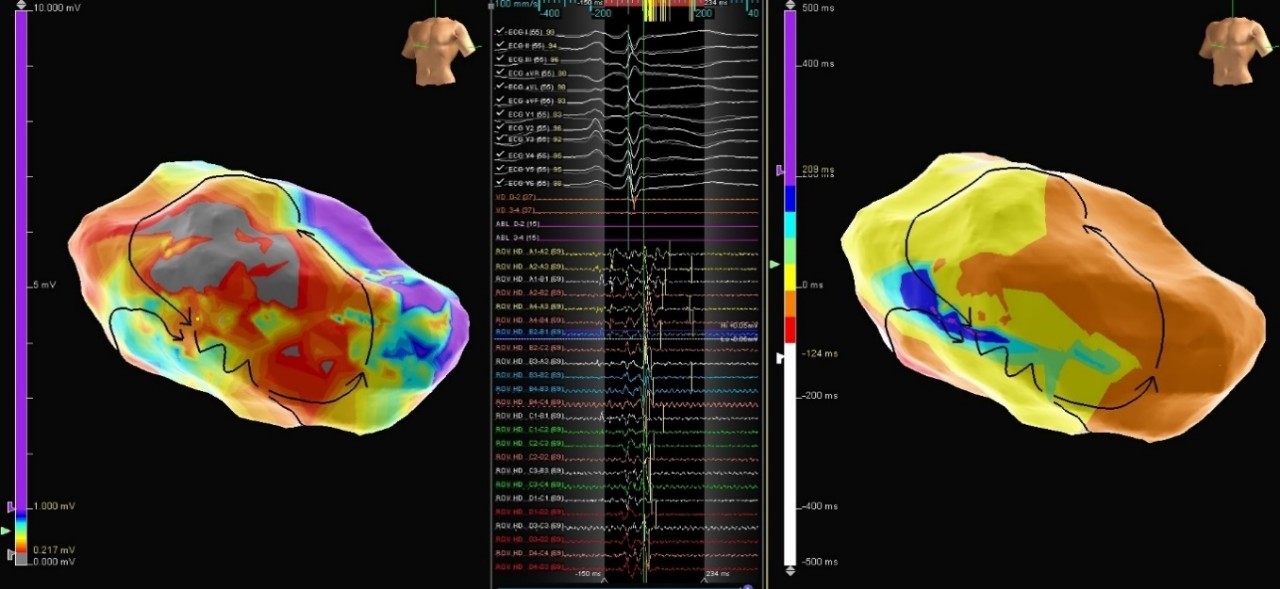
Voltage Map
VT in ARVC
Patient, diagnosed with arrhythmogenic right ventricular (RV) cardiomyopathy and ICD implantation, underwent ventricular tachycardia (VT) ablation. A voltage map in sinus rhythm was performed with the Advisor HD Grid Mapping Catheter, Sensor Enabled. Low voltages were found in the anterior and lateral wall of the RV and ILAM mapping confirmed a slow conduction zone in that area. Moreover, sustained VT was induced and mapped. A wide critical VT isthmus was found matching the ILAM map. After ablation, clinical tachycardia was no longer inducible.
Image courtesy of Dr. Naiara Calvo Galiano (Miguel Servet University Hospital | Zaragoza, Spain)
MAT-2007738 v2.0
