Greater Programming Flexibility with DeFT Response™ Technology
DeFT Response technology is Abbott-exclusive and offers the most adaptable, non-invasive programming options to rapidly optimize therapy performance to each patient’s unique needs.
With DeFT Response technology, physicians gain:
- Non-invasive programming flexibility in the management of DFTs to ensure adequate safety margins with exceptional energy delivery.
- More options for adapting to changing patient conditions following implant with or without induction testing. These options are intended to help physicians prevent fluctuations in DFTs and a diminished safety margin.1-10
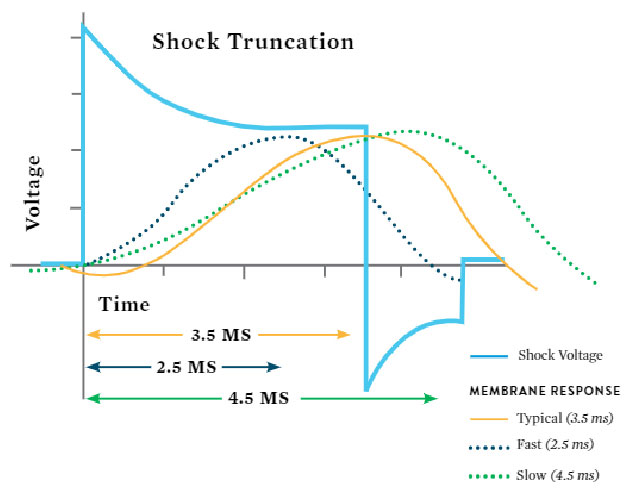
- Programmable pulse widths allow physicians to choose the duration of each phase of the shock from 2.0 ms to 6.5 ms with or without induction testing. This method lets physicians precisely match the biphasic waveform to a patient’s unique membrane response time.11-14
The physiologic variability in the patient population means that optimal truncation times are often different between individuals. By varying waveform pulsewidths, DeFT Response technology allows flexibility and patient-specific programming options.
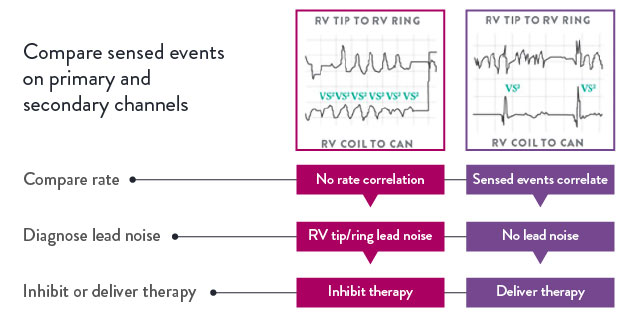
Added Protection with SecureSense RV Lead Noise Discrimination Algorithm
The SecureSense™ RV lead noise discrimination algorithm offers added protection from lead noise to reduce unnecessary therapy. It can be programmed to alert a health care professional via Merlin.net™ Patient Care Network (PCN), allowing for more rapid, clinical decision making. Programmable alerts notify the patient and clinician when lead noise is detected.
Improved Therapy Assurance
with DynamicTx
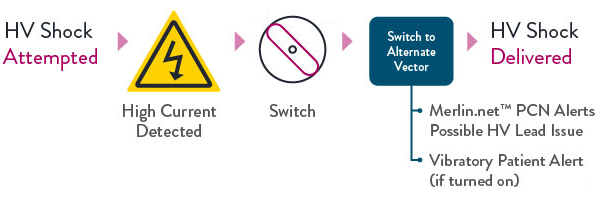
Over-Current Detection Algorithm
DynamicTx™ over-current detection algorithm is designed to provide enhanced patient safety and improved therapy assurance in the event of compromised high-voltage lead integrity, and is only available in the Abbott high-voltage portfolio.
Note
- Alternate vector options available: RV-Can and RV-SVC
- Vector switching sequence varies based on programmed configuration
Requirements
- Dual coil lead
- Programmed configuration not RV-can
References
- Shukla, H. H., Flaker, G. C., Jayam, V., & Roberts, D. (2003). High defibrillation thresholds in transvenous biphasic implantable defibrillators: clinical predictors and prognostic implications. PACE, 26(1 Pt 1), 44-48.
- Tokano, T., Pelosi, F., Flemming, M., Horwood, L., Souza, J. J., Zivin, A., . . . Strickberger, S. A. (1998). Long-term evaluation of the ventricular defibrillation energy requirement. Journal of Cardiovascular Electrophysiology, 9, 916-920.
- Wase, A., Basit, A., Nazir, R., Jamal, A., Shah, S., Khan, T., . . . McCullough, P. A. (2004). Impact of chronic kidney disease upon survival among implantable cardioverter defibrillator recipients. Journal of Interventional Cardiac Electrophysiology, 11(3), 199-204.
- Stephenson, E. A., Cecchin, F., Walsh, E. P., & Berul, C. I. (2005). Utility of routine follow-up defibrillator threshold testing in congenital heart disease and pediatric populations. Journal of Cardiovascular Electrophysiology, 16(1), 69-73.
- Nielsen, T. D., Hamdan, M. H., Kowal, R. C., Barbera, S. J., Page, R. L., Joglar, J. A. (2001). Effect of acute amiodarone loading on energy requirements for biphasic ventricular defibrillation. American Journal of Cardiology, 88(4), 446-448.
- Pelosi, F. Jr, Oral, H., Kim, M. H., Sticherling, C., Horwood, L., Knight, B. P., . . . Strickberger, S. A. (2000). Effect of chronic amiodarone therapy on defibrillation energy requirements in humans. Journal of Cardiovascular Electrophysiology, 11(7), 736-740.
- Crystal, E., Ovsyshcher, I. E., Wagshal, A. B., Katz, A., & Ilia, R. (2002). Mexiletine related chronic defibrillation threshold elevation: case report and review of the literature. PACE, 25(4 Pt 1), 507-508.
- McBride, B. F., White, C. M., Kalus, J. S., Guertin, D. C., Clyne, C. A., Baker, W. L., & Kluger, J. (2008). The impact of carvedilol on the defibrillation threshold. Heart & Lung: Journal of Acute & Critical Care, 37(1), 67-71.
- Carnes, C. A., Pickworth, K. K., Votolato, N. A., & Rarman, S. V. (2004). Elevated defibrillation threshold with venlafaxine therapy. Pharmacotherapy, 24(8), 1095-1098.
- Shinlapawittayatorn, K., Sangnoon, R., Chattipakorn, S., Suriyasataporn, W., & Chattipakorn, N. (2005). Sildenafil citrate markedly increases defibrillation threshold in swine. Journal of the American College of Cardiology, 45(3), 110A.
- Keane, D., Aweh, N., Hynes, B., Sheahan, R. G., Cripps, T., Bashir, Y., . . . Kroll, M. K. (2007). Achieving sufficient safety margins with fixed duration waveforms and the use of multiple time constants. PACE, 30(5), 596-602.
- Natarajan, S., Henthorn, R., Burroughs, J., Esberg, D., Zweibel, S., Ross, T., . . . Oza, A. (2007). “Tuned” defibrillation waveforms outperform 50/50% tilt defibrillation waveforms: a randomized multicenter study. PACE, 30(11), 1424.
- Denman, R. A., Umesan, C., Martin, P. T., Forbes, R. N., Kroll, M. W., Anskey, E. J., & Burnett, H. E. (2006). Benefit of millisecond waveform durations for patients with high defibrillation thresholds. Heart Rhythm, 3(5), 536-541.
- Mouchawar, G., Kroll, M., Val-Mejias, J. E., Schwartzman, D., McKenzie, J., Fitzgerald, D., . . . Syed, Z. (2000). ICD waveform optimization: a randomized, prospective, pair-sampled multicenter study. PACE, 23(11 Pt 2), 1992-1995.
MAT-2205139 v2.0
