Better Treatment Starts With An Accurate Diagnosis
To discover the root cause of persistent angina, patients may need an accurate diagnosis for Coronary Microvascular Dysfunction (CMD) that requires more than the angiogram alone.1 Full physiology testing of both the epicardial arteries and microcirculation can help provide a clear diagnosis to guide treatment and improve patient outcomes.2
The Microvasculature Can Have a Major Clinical and Economic Impact
The microcirculation carries far more myocardial blood volume compared to the epicardial arteries. CMD can be defined as impaired blood flow to the microcirculation, which is largely responsible for the regulation and distribution of blood flow to the myocardium.1
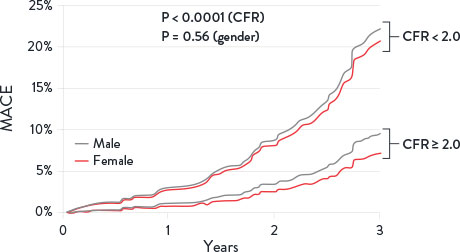
INOCA is Not Benign: The Effect On Clinical Outcomes
Patients with Ischemia and no obstructive coronary artery disease (INOCA) can be diagnosed for CMD by measuring Index of Microcirculatory Resistance (IMR) and Coronary Flow Reserve (CFR).3 Patients with abnormal CFR have an increase in major adverse cardiac events (MACE) including:
- Myocardial infarction1
- Stroke1
- Heart failure1,3
- Cardiovascular death1
Additionally, these patients have an increase in diastolic dysfunction and cardiac death.4
Coronary Flow Reserve Associated with MACE Risks1
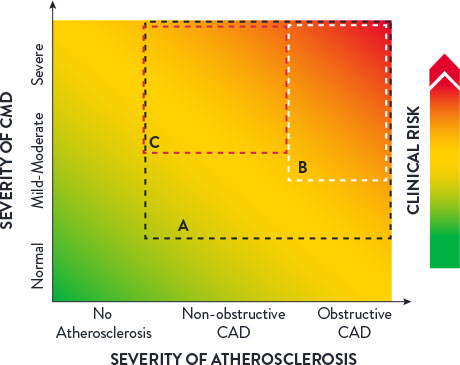
The clinical spectrum of CMD may be characterized by three factors:1
- The severity of CMD
- The degree of atherosclerosis
- Any associated clinical risks
Clinical Spectrum of CMD1
The Impact On Healthcare Costs
A clear, accurate CMD diagnosis can help reduce healthcare resource consumption.5
- For U.S. patients with INOCA symptoms, the economic cost of ineffective treatment is $13,977 per patient annually due to absenteeism (inability to go to work) and presenteeism (productivity loss at work).6
- An economic analysis of the CorMicA (CORonary MICrovascular Angina) study showed that a comprehensive physiology assessment is cost-effective compared to standard care (medical therapy and cardiac rehabilitation care) at 1-year follow-up.7
- In fact, an accurate CMD diagnosis can help reduce healthcare resource consumption,8 resulting in lower costs for hospitals and patients9 with a savings from $2,100 (Netherlands) to $7,300 (U.S.) per hospitalization avoided (2017 costs).10
INOCA Patient Identification
40-60% of all elective patients undergoing angiography suffer from INOCA. Up to half of this patient population might have angina due to CMD.11,12
- Angina post-PCI occurs in 20-30% of patients at 1-year and may be caused by CMD.13
- CMD predominantly affects women, having been detected in up to 50% of women presenting with chest pain. A definitive diagnosis is critical as women with this condition are at an increased risk of cardiovascular events in the future.14,15
Symptoms of CMD can include:16
- Discomfort in the left arm, jaw, neck, back or abdomen associated with chest pain
- Shortness of breath
- Tiredness and lack of energy
Helping Patients
The CorMicA study revealed that patients may benefit when CMD is accurately diagnosed and appropriately treated. 27% of patients saw improvement in angina severity at 1-year with optimized medical therapy.17
Sustained Angina Improvement with CMD Treatment17,†
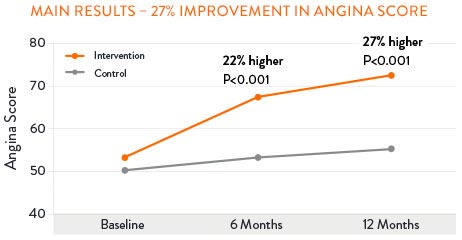
†According to the Seattle Angina Questionaire score.
Go Beyond the Angiogram with Full Physiology
The PressureWire™ X Guidewire and CoroFlow‡ Cardiovascular System is the only* One-Wire Full Physiology solution that
quantifies focal and diffuse epicardial disease and assesses
for CMD.18,19

*As compared to all commercially available Full Physiology solutions outside of the U.S. as of Q3, 2025. Refer to IFUs for additional information. Full Physiology refers to: Fractional Flow Reserve (FFR)/ Resting Full-cycle Ratio (RFR), Pullback Pressure Gradient (PPG), Index of Microcirculatory Resistance (IMR) and Coronary Flow Reserve (CFR).
References
- Taqueti, VR., et al. Coronary microvascular disease pathogenic mechanisms and therapeutic options: JACC state-of-the-art review. J Am Coll Cardiol. 2018;72:2625–2641.
- Lee, B., et al. Invasive evaluation of patients with angina in the absence of obstructive coronary artery disease. Circulation. 2015;131;10540-1060
- Gulati, MI., et al. 2021 AHA/ALL Guideline for the Evaluation and Diagnosis of Chest Pain. Circulation 2021;1440368-454.
- Knuuti, J., et al. 2019 ESC Guidelines for the diagnosis and management of chronic coronary syndromes. European Heart Journal 2020:41,407-477.
- Lee, B., et al. Invasive evaluation of patients with angina in the absence of obstructive coronary artery disease. Circulation. 2015:131:1054-1060.
- Schumann, CL., et al. Functional and economic impact of INOCA and influence of coronary microvascular dysfunction. JACC Cardiovascular Imaging 2021; 14: 1369-79.
- Heggie, R., et al. A cost-effectiveness analysis of the BHF CorMicA Trial. Interventional Journal of Cardiology 2021.
- Kunadian, V., et al. EAPCI Expert Consensus. Eur Heart J 2020;0:1-21.
- Reriani, M., et al. Coronary endothelial function testing may improve long-term quality of life in subjects with microvascular coronary endothelial dysfunction. Open Heart. 2019 6:8000870.
- Omerovic, E., et al. FFR-Guided Complete Revascularization During Primary Angioplasty: Effects on Societal Costs. EuroPCR 2017.
- Maas, A., et al. Low diagnostic yield of elective coronary angiography. The New England Journal of Medicine. 2010; 363;498.
- Maas, A. et al. Microvascular angina: diagnosis, assessment, and treatment. EMJ Int Cardiol. 2019; 7[Suppl 1]2-17.
- Jeremias, A. Post-PCI Physiology: Insights from DEFINE PCI and Other Studies. Presented at TCT 2019.
- Kuruvilla, S. & Kramer, C. MI. Coronary microvascular dysfunction in women: an overview of diagnostic strategies. Expert review of cardiovascular therapy. 2013; 11(11), 1515-1525.
- Garcia, M., et al. Cardiovascular Disease in Women: Clinical Perspectives. Circulation Research. 2016; 118(8), 1273-1293.
- Mayo Clinic webpage: Small vessel disease accessed on July 2025 at https://www.mayoclinic.org/diseases-conditions/small-vessel-disease/symptoms-causes/syc-20352117.
- Ford, TJ., et al. 1-year outcomes of angina management guided by invasive coronary function testing (CorMicA). JACC Intv. 2020;13:33-45.
- PressureWire™ X Guidewire Instructions for Use (IFU). Coroflow‡ Cardiovascular System (IFU). Refer to IFUs for additional information.
- Data on file at Abbott.
MAT-2206706 v3.0
