Angiography Doesn't Tell You The Whole Story
Approximately 112 million people globally are affected by angina and undergo coronary angiography, the primary diagnostic test for angina.1
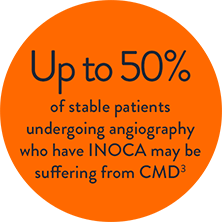
Too often patients with ischemia and no obstructive coronary artery disease (INOCA) on angiography — remain undiagnosed.2
Coronary Microvascular Dysfunction (CMD)3 is defined as impaired blood flow to the microcirculation. A clear diagnosis and optimized treatment plan can improve outcomes for these patients at high risk for major adverse cardiac events (MACE).4
How A Microvascular Dysfunction Diagnosis Benefits Patients
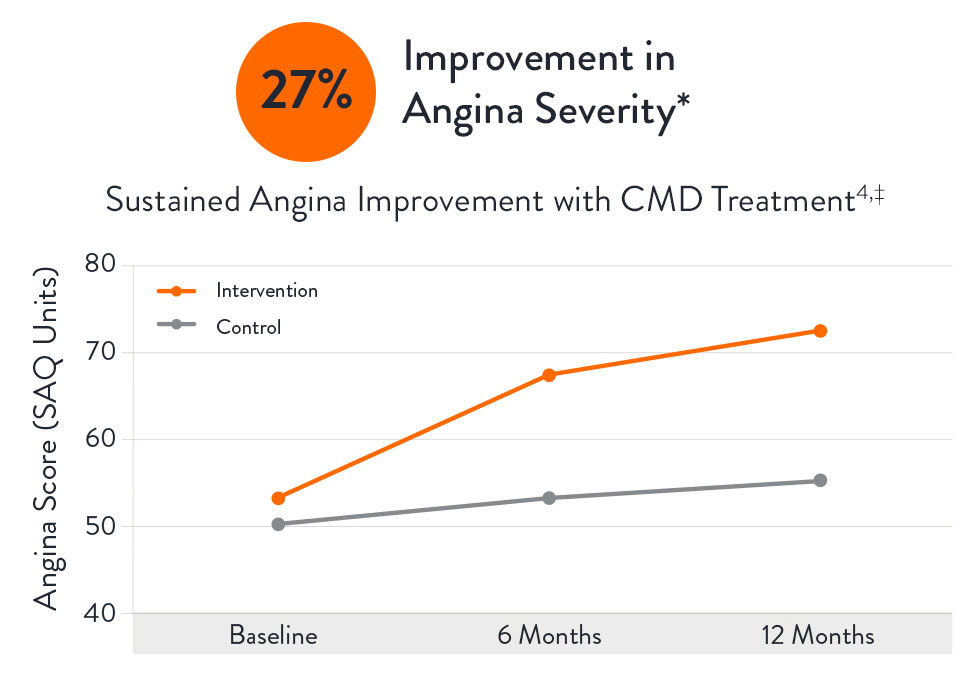
The CorMicA (CORonary MICrovascular Angina) study revealed that patients may benefit when CMD is accurately diagnosed and appropriately treated:4
- Can decrease angina severity by 27% and increase quality of life by 18%.4,6
- An accurate CMD diagnosis can help reduce healthcare resource consumption,7 resulting in lower costs for hospitals and patients8 with a savings from $2,100 (Netherlands) to $7,300 (U.S.) per hospitalization avoided (2017 costs).9
- An economic analysis of the CorMicA study showed that a comprehensive physiology assessment is cost-effective compared to standard care (medical therapy and cardiac rehabilitation care) at 1-year follow-up.10
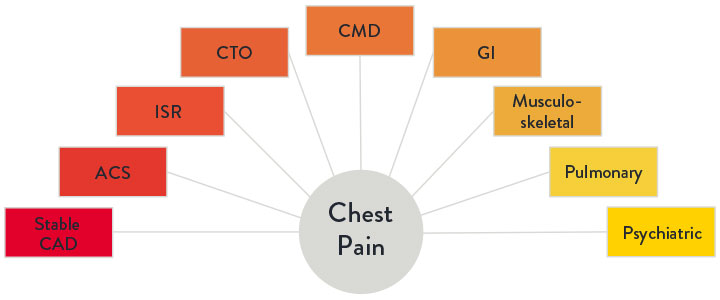
Challenges Diagnosing the Underlying Causes Of Chest Pain
Ischemic heart disease continues to be the leading cause of death globally.11 Yet chest pain—while often ischemic in nature—could have many etiologies, as illustrated.3 When chest pain is caused by ischemia, proper management depends on accurately identifying and treating the underlying cause of angina.
STRUCTURAL CAUSES7
- In-stent restenosis
- Stent thrombosis
- Progression of atherosclerotic disease in other segments
- Incomplete revascularization
- Diffuse atherosclerotic disease without focal stenosis
- Presence of myocardial bridges
FUNCTIONAL CAUSES7
- Epicardial vasospasm
- Coronary microvascular dysfunction
- Stent-related mechanical stretch of the arterial wall
The Common Diagnosis Of INOCA
Only 41% of patients assessed for angina are found to have obstructive chronic Coronary Artery Disease.13 The majority, 59% of patients, assessed for angina are found to have no angiographic abnormalities, but still have symptoms of a coronary disorder.4,5
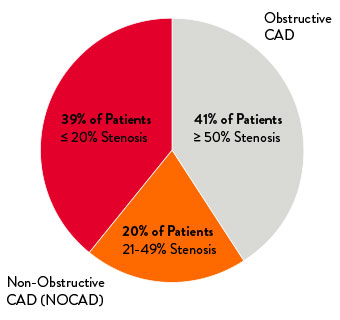
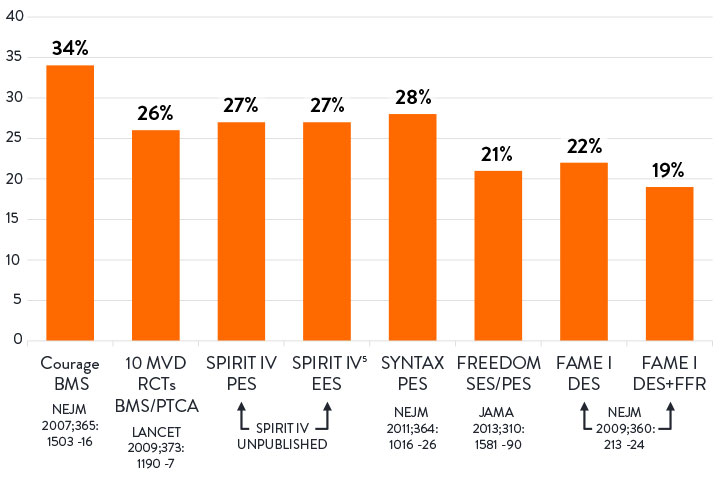
20-30% of patients experience recurrent angina in 1 year after percutaneous coronary intervention (PCI).12
Without a clear diagnosis and treatment, patients may experience recurrent hospitalizations, poor functional health, and adverse cardiovascular outcomes.7
*According to the Seattle Angina Questionnaire score.
References
- Kunadian, V. et al. An EAPCI Expert Consensus Document on Ischaemic with Non-Obstructive Coronary Arteries in Collaboration with European Society of Cardiology Working Group on Coronary Pathophysiology & Microcirculation Endorsed by Coronary Vasomotor Disorders International Study Group. European Heart Journal. 2020; 0:1-21.
- Jespersen, L. et al. Stable angina pectoris with no obstructive coronary artery disease is associated with increased risks of major adverse cardiovascular events. Eur Heart J. 2012;33:734-744.
- Marinescu, MA. et al. Coronary microvascular dysfunction and microvascular angina: a systematic review of therapies. JACC Cardiovasc Imaging. 2015;8:210-220.
- Ford, TJ. et al. 1-year outcomes of angina management guided by invasive coronary function testing (CorMicA). JACC Intv. 2020; 13:33-45.
- Patel, MR. et al. Low diagnostic yield of elective coronary angiography. N Engl J Med. 2010;362:886-895.
- Heggie, R. et al. Stratified medicine using invasive coronary function testing in angina: a cost-effectiveness analysis of the British Heart Foundation CorMicA trial. IJC. 2021.
- Lee, B. et al. Invasive evaluation of patients with angina in the absence of obstructive coronary artery disease. Circulation. 2015;131:1054–1060.
- Reriani, M. et al. Coronary endothelial function testing may improve long-term quality of life in subjects with microvascular coronary endothelial dysfunction. Open Heart. 2019;6:e000870.
- Omerovic, E. et al. FFR-Guided Complete Revascularization During Primary Angioplasty: Effects on Societal Costs. EuroPCR 2017.
- Heggie, R. et al. A cost-effectiveness analysis of the BHF CorMicA Trial. Interventional Journal of Cardiology 2021.
- Wang, H. et al. Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016;388:1459-544.
- Jeremias, A. Post-PCI Physiology: Insights from DEFINE PCI and other Studies Speaker Presentation. TCT 2019.
- Maas, A. et al. Microvascular angina: diagnosis, assessment, and treatment. EMJ Int Cardiol. 2019; 7[Suppl 1]2-17.
MAT-2002360 v5.0
