MAT-2105201 v1.0
What is Coronary Microvascular Dysfunction (CMD)?
Angiography Doesn’t Tell You The Whole Story
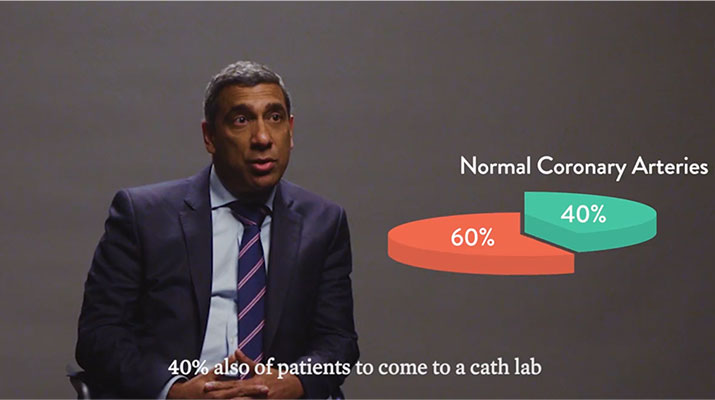
Angina is a condition that affects over 112 million people around the world.1 Many patients with angina undergo coronary angiography to assess the epicardial arteries and identify the root cause of angina.1 Unfortunately, angiography cannot assess the microcirculation—responsible for much of the regulation and distribution of blood flow to the myocardium.2 This means the majority (59%) of patients assessed for angina are found to have no angiographic abnormalities, but still have symptoms of a coronary disorder.3,4
Additionally, 20-30% of patients continue to experience persistent angina even after percutaneous coronary intervention (PCI), making repeat visits to the cardiologist’s office, where a lack of a clear diagnosis can make it difficult to determine a clear plan for disease management. These patients with ischaemia and no obstructive coronary artery disease (INOCA) and/or post-PCI angina may be suffering from Coronary Microvascular Dysfunction (CMD),5 defined as impaired blood flow to the microcirculation.2
Why should you care about CMD?
Hear Prof. Divaka Perera, a consultant cardiologist from London, UK, discuss why measuring microvascular function for CMD can improve patient management.
INOCA's Impact on Clinical Outcomes
INOCA is not benign2 or a final diagnosis. Up to 50% of stable patients undergoing angiography have INOCA who may be suffering from CMD.4
Patients with INOCA, including those diagnosed with CMD, have an increase in major adverse cardiac events (MACE) including:
- Myocardial infarction6
- Stroke6
- Heart failure2,6
- Cardiovascular death6
Additionally, these patients have an increase in diastolic dysfunction and cardiac death.2
Coronary Flow Reserve Associated with MACE Risks2
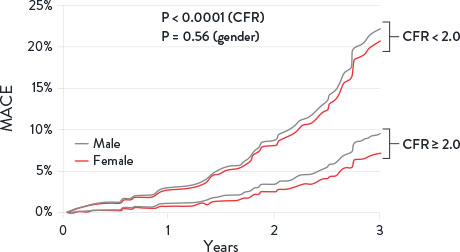
CMD is defined by cardiac positron emission tomography/ computed tomography CF < 2 in patients without overt obstructive coronary artery disease. MACE = Major Adverse Cardiovascular Events. Image adapted from Taqueti et al. J Am Cardiol. 2018²
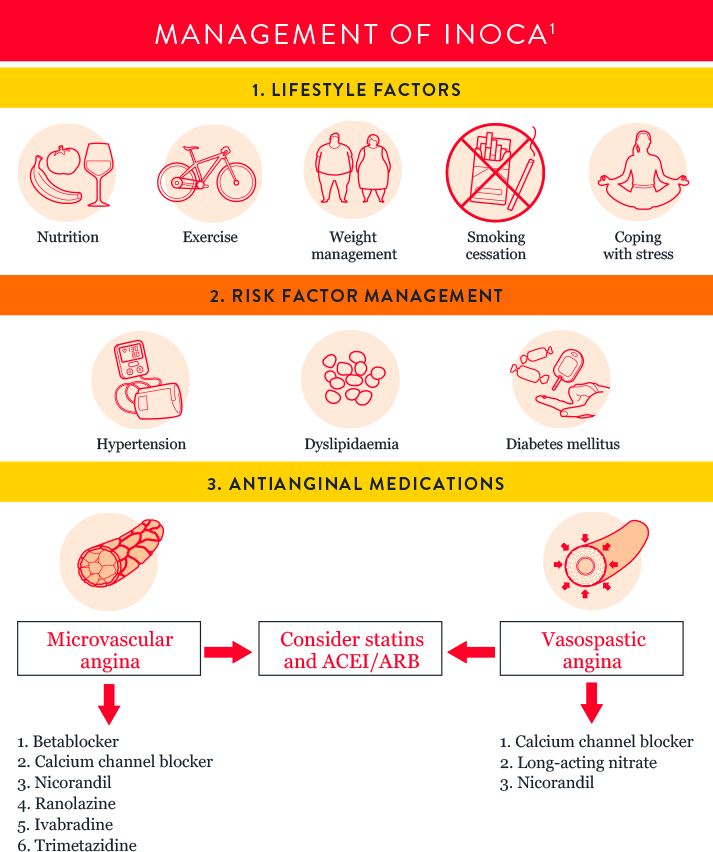
INOCA Endotype Evaluation and Management Guidelines
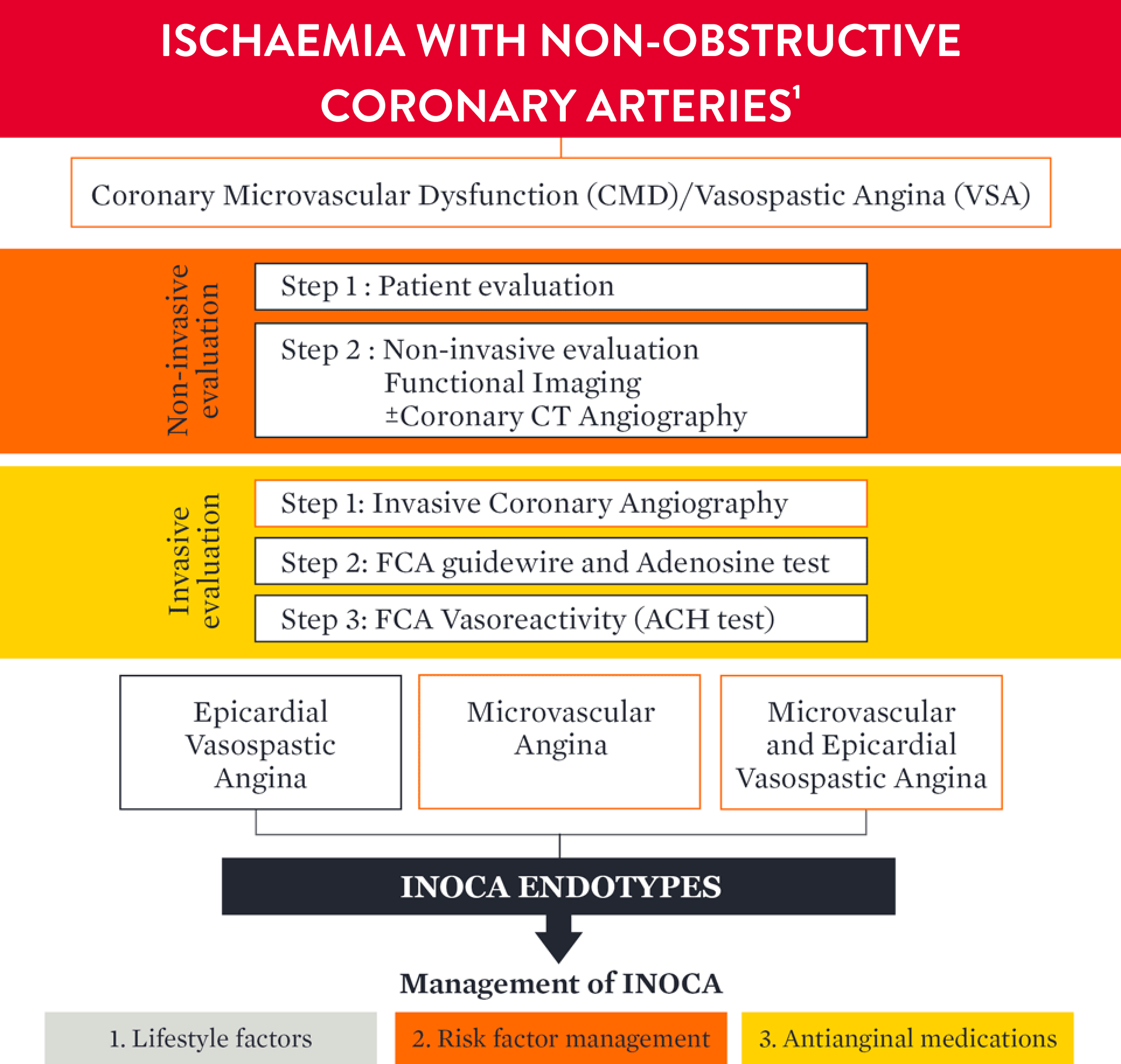
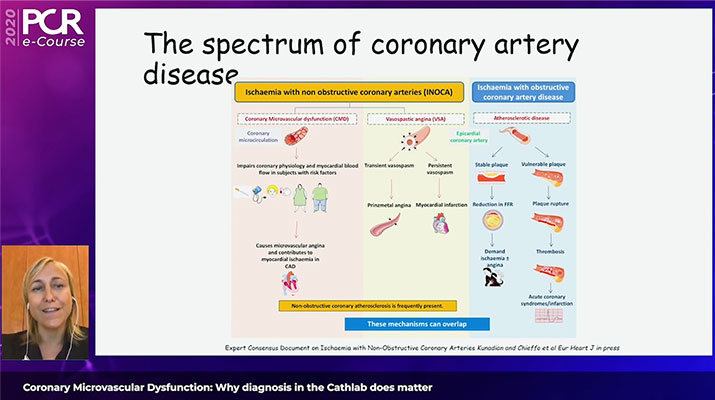
Watch the video below to hear Dr. Aladie Chieffo discuss the work-up for INOCA patients to determine a CMD diagnosis.
Aladie Chieffo MD, Milan, Italy
References
- Kunadian, V., et al. An EAPCI Expert Consensus Document on Ischaemic with Non-Obstructive Coronary Arteries in Collaboration with European Society of Cardiology Working Group on Coronary Pathophysiology & Microcirculation Endorsed by Coronary Vasomotor Disorders International Study Group. European Heart Journal. 2020;0:1-21.
- Taqueti, VR., et al. Coronary microvascular disease pathogenic mechanisms and therapeutic options: JACC state-of-the-art review. J Am Coll Cardiol. 2018;72:2625–2641.
- Patel, M, et al. Low diagnostic yield of elective coronary angiography. N Engl J Med. 2010;362:11.
- Marinescu, MA., et al. Coronary microvascular dysfunction and microvascular angina: a systematic review of therapies. JACC Cardiovasc Imaging. 2015;8:210-220.
- Jeremias, A. et al. Blinded Physiological Assessment of Residual Ischemia After Successful Angiographic PCI. JACC Cardiovascular Intervent. 2019;12(20).
- Jespersen, L., et al. Hvelplund A, Abildstrøm SZ, et al. Stable angina pectoris with no obstructive coronary artery disease is associated with increased risks of major adverse cardiovascular events. Eur Heart J. 2012;33:734-744. doi:10.1093/eurheartj/ehr331.
MAT-2414037 V1.0