DeFT Response technology offers the most highly adaptable, non-invasive programming options to rapidly optimize therapy performance to each patient’s unique needs.
DeFT Response technology is only available in Abbott high-voltage devices.
With DeFT Response technology, physicians gain:
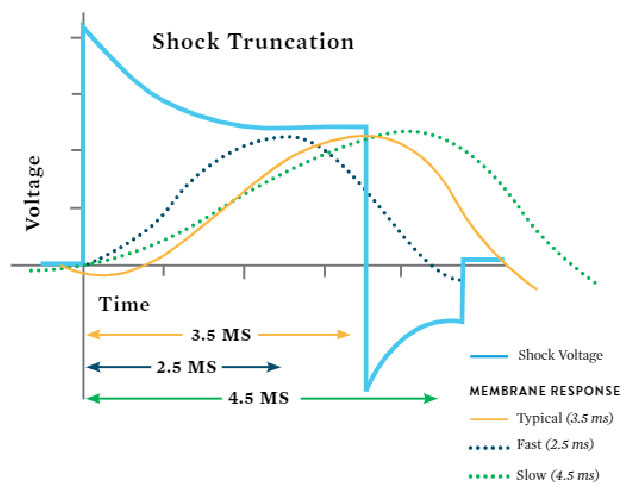
The physiologic variability in the patient population means that optimal truncation times are often different between individuals. By varying waveform pulse widths, DeFT Response technology allows flexibility and patient-specific programming options.
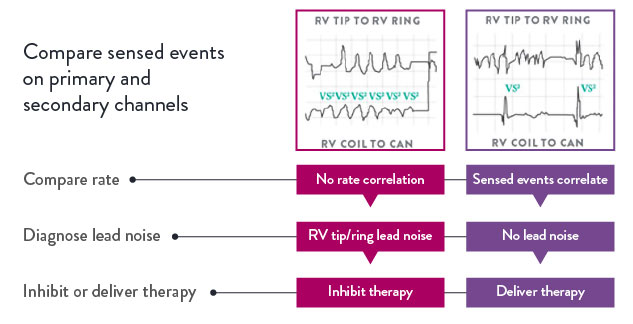
The SecureSense RV lead noise discrimination algorithm offers added protection from lead noise to reduce unnecessary therapy. It can be programmed to alert a health care professional via Merlin.net™ Patient Care Network (PCN), allowing for more rapid, clinical decision making. Programmable alerts notify the patient and clinician when lead noise is detected.
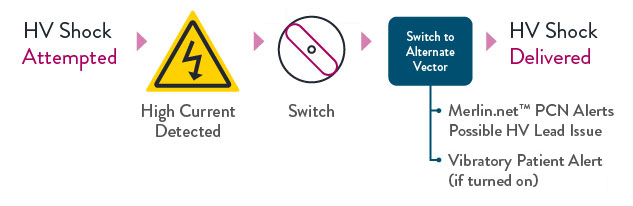
DynamicTx over-current detection algorithm is designed to provide enhanced patient safety and improved therapy assurance in the event of compromised high-voltage lead integrity, and is only available in the Abbott high-voltage portfolio.
Note
Requirements
More than 10 years of data from the industry's largest, prospective, actively monitored registry studies confirms the reliability of high-voltage leads with Optim™ lead insulation.
In addition, studies have confirmed the abrasion resistance and biostability of Optim lead insulation:
MAT-2009580 v2.0
STAY CONNECTED