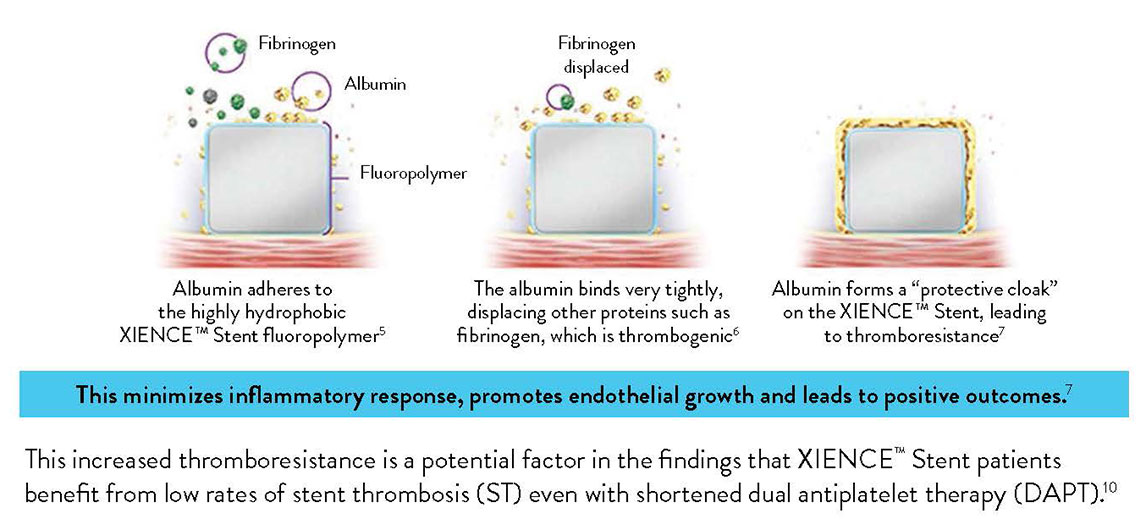
The XIENCE™ Stent polymer with a fluorinated surface has shown protective attributes—the ability to tightly bind albumin to create a “protective cloak” around the stent.2
Another factor that sets XIENCE™ Stent apart is its fluoropolymer coating. Unlike other polymer coatings, the fluoropolymer interacts with proteins in the blood in a way that reduces thrombus formation—a process known as fluoropassivation.
XIENCE™ Stent, widely considered to be the gold standard for patient safety and efficacy, is coated with a fluoropolymer.
THE XIENCE™ STENT FLUOROPOLYMER: PROVEN TO PROTECT
Due to thromboresistance and low inflammatory responses, fluorinated surfaces encourage faster endothelization and healing.4
Moreover, the XIENCE™ Stent fluoropolymer has minimal coating defects compared to biodegradable polymer DES (BP-DES).9
In contrast to the visual above, most stents available today—biodegradable polymer stents, durable polymer stents or bare metal stents—have non-fluorinated surfaces that interact with proteins in the following ways:
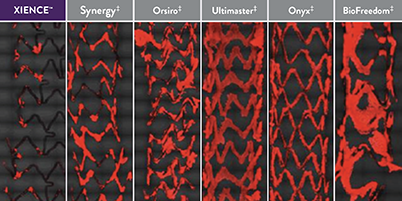
XIENCE™ Stent’s fluoropolymer demonstrates the fewest platelets adhering to the stent surface—an important factor in stent thrombosis.3 This fluoropolymer can protect patients from both acute and long-term complications.3,13
Representative confocal photomicrographs stained for platelets (CD42b/CD61). N=5 per stent. This preclinical ex vivo porcine shunt model used aspirin-only antiplatelet therapy.
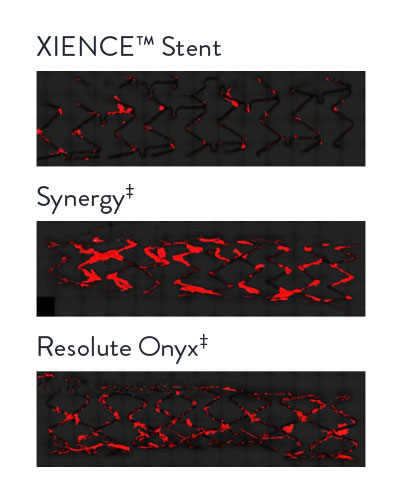
Representative confocal photomicrographs stained for platelets (CD42b/CD61). N=8 per stent. This preclinical ex vivo porcine shunt model used clopidogrel-only antiplatelet therapy.
In the images “on the right you can see the [pro-thrombotic] platelet adherence. XIENCE™ Stent [the image at the bottom] has hardly any attachments to it.” — Renu Virmani, MD, referring to the photomicrographs, where green indicates platelet adhesion.
In several analyses, XIENCE™ Stent exhibits the most thromboresistance when compared to several different BP-DES.3,14
Ex vivo porcine photomicrographs reveal the least thrombus area on XIENCE™ Stent (green areas are platelets).
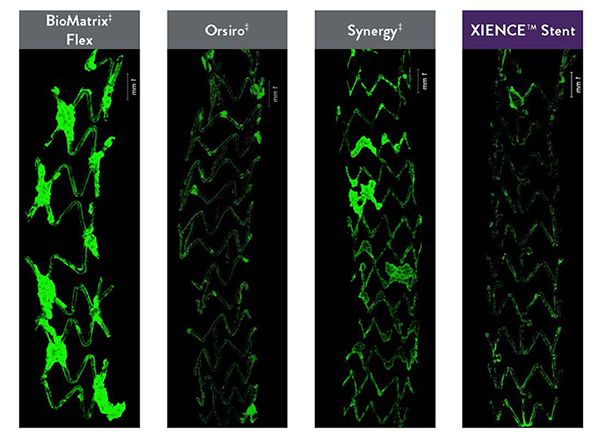
CVPath Institute also conducted tests to show real-time platelet-device interaction between different types of stents.
This preclinical model used in vitro human blood with heparin only. Representative confocal photomicrographs stained for platelets. Real-time platelet-device interaction was visualized under confocal microscopy and recorded in a time-lapse video. Image processing quantified platelet deposition on devices.
MAT-2101781 v2.0
You are about to enter an Abbott country- or region-specific website.
Please be aware that the website you have requested is intended for the residents of a particular country or countries, as noted on that site. As a result, the site may contain information on pharmaceuticals, medical devices and other products or uses of those products that are not approved in other countries or regions
Do you wish to continue and enter this website?
MAT-2305078 v1.0